- 1Centre for Health Management and Policy Research, School of Public Health, Cheeloo College of Medicine, Shandong University, Jinan, China
- 2National Health Commission of China Key Lab for Health Economics and Policy Research (Shandong University), Jinan, China
- 3The Sixth People Hospital of Hebei Province, Baoding, China
Objectives: We want to test the association between carbon monoxide poisoning (CMP) experiencing and lifetime suicidal ideation/suicide plan among community residents.
Methods: This is a population-based cross-sectional study conducted among community residents in Hebei province, China. We analyzed a total of 21,376 valid questionnaires. CMP experience and lifetime suicidal ideation/suicide plan were assessed in this study. Logistic regression and false discovery rate correction were conducted to analyze the associations and correct the p values.
Results: We found that CMP (OR = 2.56, p < 0.001, corrected-p = 0.001) was associated with lifetime suicidal ideation, and the other risk factors were female (OR = 0.53, p < 0.001, corrected-p = 0.001). The association between CMP and suicide plan was not supported after false discovery rate correction (OR = 2.15, p = 0.035, corrected-p = 0.385). For the CMP patients, experiencing ≥2 times CMP (OR = 2.76, p = 0.001, corrected-p = 0.011) was also in higher risk of lifetime suicidal ideation. The association between CMP times and lifetime suicidal plan was not supported after false discovery rate correction (OR = 4.95, p = 0.021, corrected-p = 0.231).
Conclusion: CMP patients are in higher risk of lifetime suicidal ideation. For CMP patients, some strategies are needed to control their suicidal ideation.
Introduction
According to the latest estimates by World Health Organization (WHO), there were more than 700,000 people died by suicide in 2019, which meant that one in 100 deaths was caused by suicide, and the number of death caused by suicide was also higher than HIV, malaria, breast cancer, war or homicide [1]. In China, although the suicide rates decreased in the recent years [2], suicide was also the top 10 causes of death [3]. All of these informed us that suicide was an important public health and society problem in China and some other countries worldwide.
Carbon monoxide poisoning (CMP), mainly caused by accidences [4, 5], was a frequent cause of acute toxicity with high morbidity and mortality worldwide [6, 7]. Previous studies had found that nervous system disorders, including sleep initiation and maintenance disorders, tension-type headache, occur in over half of the patients within the first years after CMP [8]. In recent years, several longitudinal studies also supported that sleep disorders can be warning signs for imminent suicidal thought and behaviors [9–11]. Basing on these longitudinal findings, we have reasons to assume the association between CMP and suicidal thought and behaviors, including suicidal ideation and suicide plan.
In the other sides, the central nervous system was the most frequently affected by CMP, and most of the frequent outcomes of CMP were delayed neuropsychiatric sequelae, such as delayed encephalopathy [12, 13]. Patients with delayed neuropsychiatric sequelae would have changes on individual’s mental status and behaviors [14–16]. As one kind of individual’s behaviors, suicide may also be associated with the changes of mental status and behaviors. Although the mechanism for this relationship was not clear until now [17], cognitive decline may be one of the explanations for this association, which is also a risk factor for suicidal ideation [18–20]. Actually, some publications also reported that there was nucleotide variation in central nervous system genes for suicide risk [21, 22]. In practice, there were also several case studies, which reported several cases conducted suicide after CMP. One was a truck driver, and he committed suicide 15 months later after CMP [23]. Another case was a 12-year-old girl, who also conducted suicide after CMP [24]. However, to our knowledge, this association between CMP and suicidal ideation was not tested in the population level until now.
To fill the gap, we conducted a population-based cross-sectional study to test the association between CMP and suicidal ideation/suicide plan. As two kinds of suicidal behaviors, suicidal ideation and suicide plan had been proved to be an important predictor for the following suicidal behaviors [25, 26], which should be paid more attentions. Establishing the associations between CMP and suicidal ideation/suicide plan is also helpful for us to further understand the suicidal behaviors and the impact of CMP. If the association can be identified, the findings not only remind our attention on the nature and the pathogenesis of CMP, but also draw us the further strategies to control suicidal ideation, especially for the clinicians.
Methods
Study Sample and Design
This study was conducted in Chinese Hebei province from June to August 2018 with a cross-sectional design. Hebei located in the north of China, and its Gross Domestic Product (GDP) ranked 9th in all the 31 provinces of Chinese mainland [27]. To make sure the representativeness of the sample, a three-stage multistage stratified cluster sampling was used to select the community residents aged 18 years and above. First, five cities (Shijiazhuang, Baoding, Xingtai, Zhangjiakou, Qinhuangdao) were randomly selected from all the 11 cities in Hebei. Second, we randomly selected three counties (rural region) and one district (urban region) in each selected city. Third, one township or sub-district was randomly selected from each county or district. Fourth, we randomly selected one village (community) in each selected township (sub-district). Totally, we selected 15 rural villages and 5 urban communities to conduct the study’s survey. Residents aged 18 years and above in the selected villages or communities were interviewed in this study. Finally, 21,376 valid questionnaires were analyzed to get the association between carbon monoxide poisoning and suicidal ideation.
Interviewing Procedures
Before the survey, the research group trained all the interviewers for 2 days to make sure they had fully understood the research and questionnaire. After the training, a face-to-face interview was scheduled by one interviewer for all the participants upon their agreement with written informed consent form. To ensure the quality of the questionnaire, all the questionnaires were checked by other reviewer on each interview day. For the questionnaires with missing data or logical problems, the interviewers were asked to revisit or call the interviewees on the next day. The study protocol was approved by the Institutional Review Board (IRB) of Hebei Mental Health Center before data collection. Written informed consent was obtained from all the participants.
Measures
Lifetime Suicidal Ideation and Plan
Lifetime suicidal ideation was assessed by the question that “whether you ever seriously thought about killing yourself?” The answer can be chosen from yes (1) or no (0). For the people with positive answers, they would be asked that whether they ever made a plan for suicide. Participants who chose yes were seen as experiencing suicidal ideation or plan. These questions were used to assess suicidal ideation and plan in many previous studies, such as United States National Comorbidity Survey (NCS), National Comorbidity Survey Replication (NCSR) [28] and many other studies worldwide [29, 30].
Lifetime Carbon Monoxide Poisoning Experience and Its Times
Lifetime carbon monoxide poisoning (CMP) experience was evaluated by the question that “have you ever experienced carbon monoxide poisoning?” The answers were also yes (1) and no (0). Subjects who answered yes were analyzed as experiencing CMP. For people who experienced CMP, we further asked the times for their CMP experiencing. As there were few subjects experienced CMP more than 2 times, we recoded it into 1 time (0) and ≥2 times (1).
Social-Demographic Variables
Gender was evaluated by male (1) or female (0). Age was calculated by the participants’ date of birth. Ethnicity was evaluated by Han (1) and others (0). Education level was assessed by the participants’ academic degree with the 4 options, less of elementary (1), elementary school (2), middle school (3) and high school or above (4). Married status was evaluated through one question about the participants’ married status. The answers were never married, married, divorced, widowed, deuterogamist, and others. As the small percentage of the last four answers, we recoded it into unmarried (1), married (2), and others (3). Region was assessed by asking the region where the participants lived, and the answers contained urban (0) and rural (1). Living alone was evaluated by number of people lived with the participants. For participants lived without other persons were recoded into living alone (1), and others were recoded into not living alone (0).
Statistical Methods
SPSS for Windows 24.0 (web version) and R (version 4.2.0) were used to conduct the data analysis. Student’s t-test or Chi-square test was performed to compare the means or proportions between social-demographic variables, CMP experiencing (times), and suicidal ideation/suicide plan. Logistic regression was performed to examine the association between CMP experiencing (times) and suicidal ideation/suicide plan after controlling social-demographic variables. False discovery rate correction with Benjamini-Hochberg method was further performed to correct the p values of logistic regressions. All significance tests were two-tailed, and a p-value of 0.05 or lower was considered as statistical significance.
Results
In this study, we interviewed a total of 21,376 participants aged 18 years and above among community residents in Hebei province, China. The prevalence of lifetime suicidal ideation and suicide plan was 1.4% (289/21,376) and 0.3% (67/21,376), respectively. In Table 1, we descripted the sample characteristics. In this sample, there were 11,537 females (54.0%) and 9,839 males (46.0%), and the mean age was 50.85 years. The detailed information could be found in the second column of Table 1. We also analyzed the factors associated with lifetime suicidal ideation, and the risk factors were female (
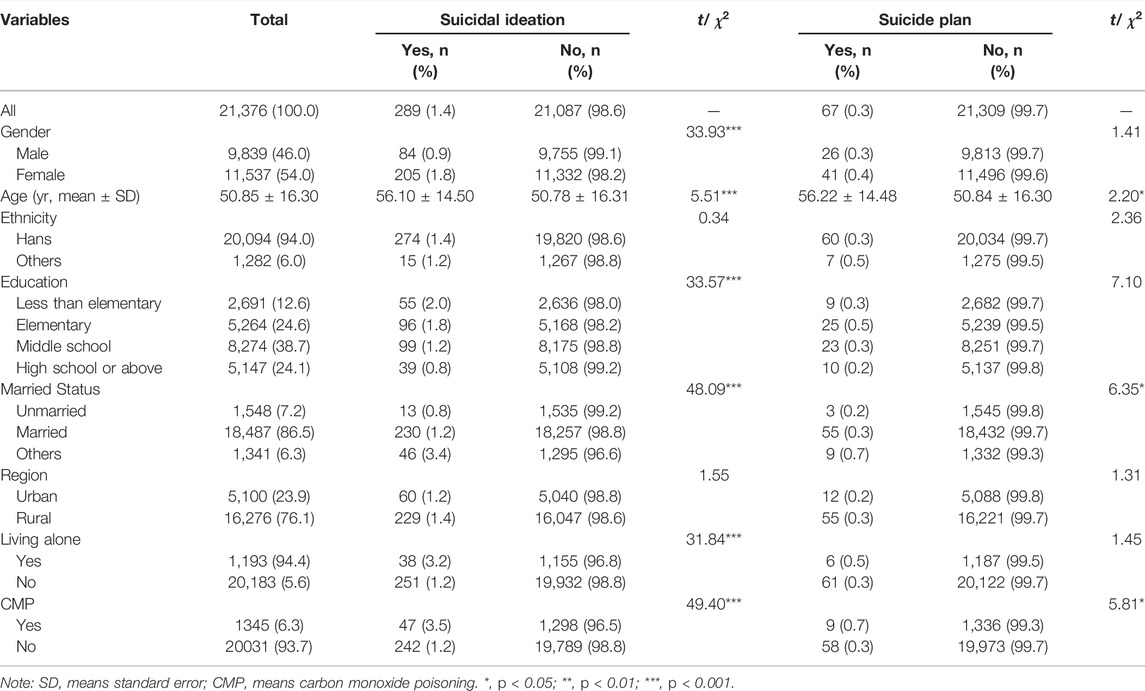
TABLE 1. Sample description and single analysis between social-demographic variables, carbon monoxide poisoning and suicidal ideation/suicide plan (Hebei, China. 2018).
In Table 2, logistic regressions were conducted to analyze the factors associated with lifetime suicidal ideation/suicide plan, and false discovery rate correction with Benjamini-Hochberg method was also performed to correct the p values. The results of logistic regression supported that the risk factors of lifetime suicidal ideation were female (OR = 0.54, p < 0.001), older age (OR = 1.01, p = 0.029), elementary education (OR = 1.77, p = 0.007), not being married (OR = 0.59, p = 0.015), and CMP experience (OR = 2.56, p < 0.001). After the false discovery rate correction, female (corrected-p = 0.001), elementary education (corrected-p = 0.026), not being married (corrected-p = 0.041), and CMP experience (corrected-p = 0.001) were positively associated with lifetime suicidal ideation. For lifetime suicide plan, CMP experience (OR = 2.15, p = 0.035) was the only risk factor associated with suicide plan. After false discovery rate correction, the association between CMP experience and suicide plan disappeared (corrected-p = 0.385). The detailed information can be found in Table 2.
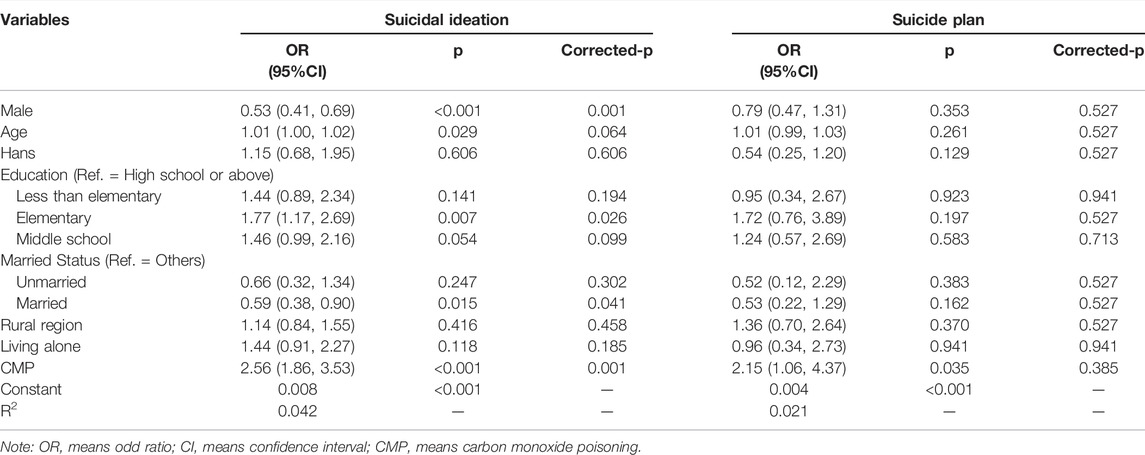
TABLE 2. Logistic regressions for the associations between social-demographic variables, carbon monoxide poisoning, and suicidal ideation/suicide plan (Hebei, China. 2018. n = 21,376).
As the findings about the significant association between CMP and lifetime suicidal ideation, we further analyzed the association between CMP times and lifetime suicidal ideation/suicide plan. In the whole sample, there were 6.3% (1,345/21,376) of the participants experienced CMP in their lives. We firstly analyzed the sample characteristics for the people who ever experienced CMP, which was shown in the second column of Table 3. For people who ever experienced CMP, there were 19.2% (258/1345) of them experienced CMP 2 or more times. The results showed that CMP times were positively associated with lifetime suicidal ideation (
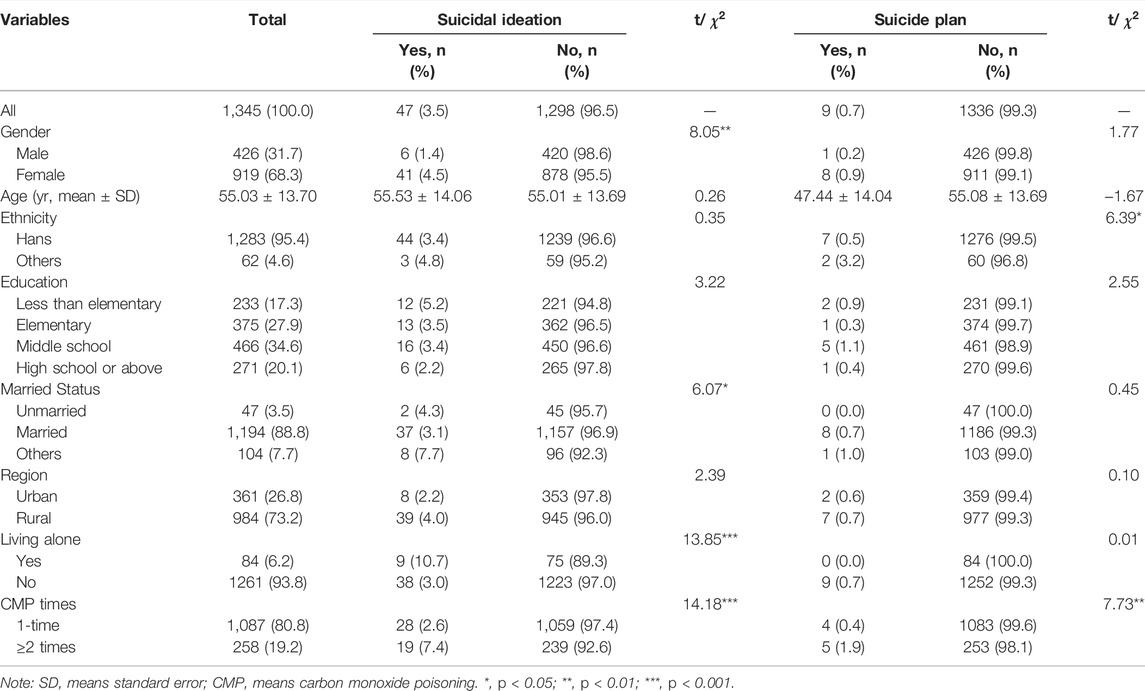
TABLE 3. Sample description and single analysis between social-demographic variables, carbon monoxide poisoning times and suicidal ideation/suicide plan among people experienced carbon monoxide poisoning (Hebei, China. 2018).
In Table 4, logistic regressions were also conducted to analyze the association between CMP times and lifetime suicidal ideation/suicide plan among people ever experienced CMP. The results showed that female (OR = 0.35, p = 0.022), living alone (OR = 3.90, p = 0.014), and more CMP times (OR = 2.76, p = 0.001) was positively associated with lifetime suicidal ideation. After false discovery rate correction, only more CMP times (corrected-p = 0.011) was positively associated with lifetime suicidal ideation. For lifetime suicide plan, we found that the risk factors were more CMP times (OR = 4.95, p = 0.021). The association between CMP times and lifetime suicidal plan was not supported after false discovery rate correction (corrected-p = 0.231). The detailed information was shown in Table 4.
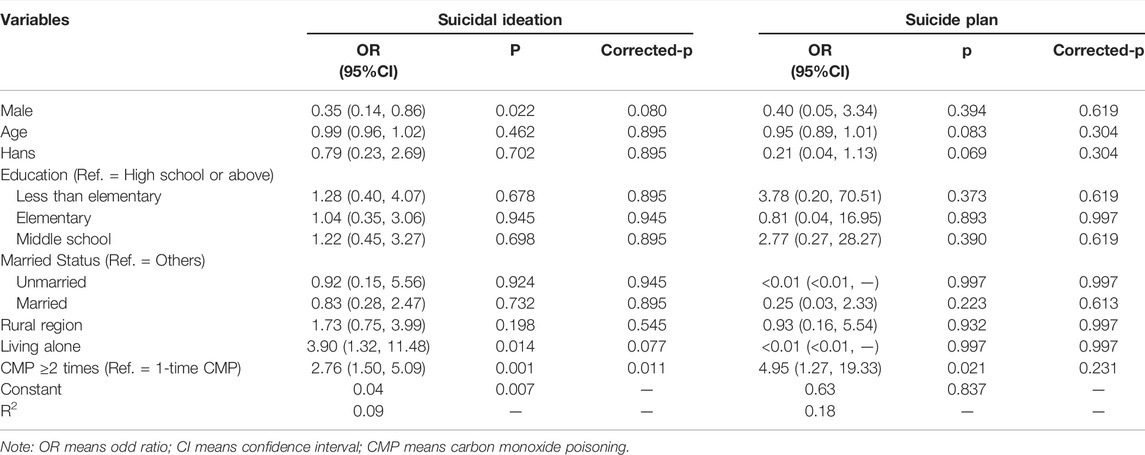
TABLE 4. Logistic regressions for the associations between social-demographic variables, carbon monoxide poisoning times, and suicidal ideation/suicide plan among people experienced carbon monoxide poisoning (Hebei, China. 2018. n = 1,345).
Discussion
In this study, we mainly want to analyze the relationship between CMP and suicidal ideation/suicide plan, and the results supported the associations between CMP and suicidal ideation based on a population-based cross-sectional design. The associations between CMP times and suicidal ideation were also analyzed in this study, and the results supported that people ever experienced two or more times CMP were in higher risk of suicidal ideation, comparing with subjects experienced only 1-time CMP. Our results also found that CMP experience and more CMP times were positively associated with suicide plan, but both the associations would be disappeared after false discovery rate correction.
The first aim for this study was to explore the association between CMP and suicidal ideation/suicide plan, and we found that people who experienced CMP were in higher risk of suicidal ideation. To our knowledge, this is the first population study, which reported this relationship. One of the explanations for this relationship was about the neuropsychiatric sequelae after CMP. As we introduced in the Introduction section, people who experienced CMP may have several neuropsychiatric sequelae, such as sleep problems, cognitive decline, chronic pain, and so on [8, 31]. All of these sequelae of CMP were risk factors for suicidal ideation, which had been identified in previous studies [32, 33]. The association between CMP and suicide plan was not supported after false discovery rate correction. It may be explained by the small sample of suicide planner experienced CMP. In this study, although we interviewed more than 20,000 residents, only 9 of them experienced CMP had made suicide plans.
The other finding was about the association between CMP times and suicidal ideation/suicide plan among participants who experienced CMP. Our results supported that people who experienced two or more times CMP were in higher risk of suicidal ideation, and the association between CMP times and suicide plan was not supported after false discovery rate correction. These findings further implied us the associations between CMP and suicidal ideation. Similar to the association between CMP experience and suicidal ideation. The reasons also can be explained by the sequelae of CMP. For people who experienced more times CMP, they might suffer more severe and frequent sequelae of CMP, which were risk factors for suicidal ideation. For the association between CMP times and suicide plan, our results did not support the association between more CMP times and suicide plan after false discovery rate correction. It also could be explained by the small sample of suicide planner experienced CMP. In this study, only 5 residences experienced 2 or more times of CMP.
In this study, the prevalence of suicidal ideation and suicide plan was 1.4% and 0.3%, respectively. For suicidal ideation, the prevalence was varied from 1.1% to 22.5% in different studies [34–36]. The prevalence of suicide plan was also ranged from 0.7% to 15.6% [37–39]. Our results (1.4% and 0.3%) are lower than the previous findings. It may be caused by the regions of the research. Most the publication about Chinese suicidal ideation was interviewed in Chinese metropolitan [26, 40, 41], and our study was conducted in general urban and rural regions. People live in Chinese metropolitan have higher work stress, and they may report higher suicidal ideation than others [42–44]. The other reason may be caused by the decreased suicide rates in China, especially in rural China [45]. For the prevalence of CMP, to our knowledge, there is no population study, which reported this prevalence among community residents, and we cannot compare it with other studies.
In this study, we also found some other risk factors associated with suicidal ideation, such as male, lower education. Actually, all of these control variables have been identified in previous studies. For the gender differences, females are in higher risk of suicidal ideation worldwide [39, 46], but they are in lower risk of suicide death in many countries except China and a few countries [1, 47]. The positive associations between lower education and suicidal ideation/suicide plan were also proved in many studies [11, 29, 48–50].
There are some limitations, which should be considered when we explain the findings. First, this is a cross-sectional study, and we did not interview the temporal orders of CMP and suicidal ideation. Both of them resulted we could not get any causal relationships for the association between CMP and suicidal ideation. Second, the lifetime CMP experience, lifetime suicidal ideation and other control variables were evaluated by the participants’ self-report, and the recall bias cannot be avoided. Third, as we know, CMP is also a method for suicidal behaviors. Although the percentage of suicide by CMP is in a very low level [51, 52], it may also cause some bias for the findings in this study because of the hard works about distinguishing the suicide ideators or planers from suicide attempters using CMP in this study. Forth, this study did not test the inter-rater agreement, and it may also cause some bias for the findings in this study.
Despite these limitations, this is the first population study, which reported the association between CMP, suicidal ideation and suicide plan. The results also remind us that experiencing of CMP can increase the risk of suicidal ideation, and it also implies the effect of CMP on individuals’ behaviors, which can be explored in the future studies. For people experienced CMP, close family and psychiatric follow-up are important and needed to control their suicidal ideation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of Hebei Mental Health Center. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
All authors read and approved the final manuscript. LS analyzed the data and wrote the draft. KL and LZ commented on the manuscript. YZ designed the study and commented on the draft of this manuscript.
Funding
The authors declare that this study received funding from the National Natural Science Foundation of China (71603149 and 71974114). The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.WHO. Suicide Worldwide in 2019: Global Health Estimates. Geneva: World Health Organization (2021).
2. Zhang, J, Sun, L, Liu, Y, and Zhang, J. The Change in Suicide Rates between 2002 and 2011 in China. Suicide Life Threat Behav (2014) 44(5):560–8. doi:10.1111/sltb.12090
3. Sun, L, and Zhang, J. Potential Years of Life Lost Due to Suicide in China, 2006-2010. Public Health (2015) 129(5):555–60. doi:10.1016/j.puhe.2015.02.012
4.Centers for Disease Control and Prevention. Outdoor Carbon Monoxide Poisoning Attributed to Tractor exhaust--Kentucky, 1997. MMWR Morb Mortal Wkly Rep (1997) 46(51):1224–7.
5. Al-Matrouk, A, Al-Hemoud, A, Al-Hasan, M, Alabouh, Y, Dashti, A, and Bojbarah, H. Carbon Monoxide Poisoning in Kuwait: A Five-Year, Retrospective, Epidemiological Study. Int J Environ Res Public Health (2021) 18(16):8854. doi:10.3390/ijerph18168854
6. Sadovnikoff, N, Varon, J, and Sternbach, GL. Carbon Monoxide Poisoning. An Occult Epidemic. Postgrad Med (1992) 92(4):86–96. doi:10.1080/00325481.1992.11701467
8. Rhee, B, Kim, H-H, Choi, S, and Min, YG. Incidence Patterns of Nervous System Diseases after Carbon Monoxide Poisoning: A Retrospective Longitudinal Study in South Korea from 2012 to 2018. Clin Exp Emerg Med (2021) 8(2):111–9. doi:10.15441/ceem.20.099
9. Harris, LM, Huang, X, Linthicum, KP, Bryen, CP, and Ribeiro, JD. Sleep Disturbances as Risk Factors for Suicidal Thoughts and Behaviours: A Meta-Analysis of Longitudinal Studies. Sci Rep (2020) 10(1):13888. doi:10.1038/s41598-020-70866-6
10. Bernert, RA, Turvey, CL, Conwell, Y, and Joiner, TE. Association of Poor Subjective Sleep Quality with Risk for Death by Suicide during a 10-year Period: A Longitudinal, Population-Based Study of Late Life. JAMA Psychiatry (2014) 71(10):1129–37. doi:10.1001/jamapsychiatry.2014.1126
11. Liu, RT, Steele, SJ, Hamilton, JL, Do, QBP, Furbish, K, Burke, TA, et al. Sleep and Suicide: A Systematic Review and Meta-Analysis of Longitudinal Studies. Clin Psychol Rev (2020) 81:101895. doi:10.1016/j.cpr.2020.101895
12. Han, S, Choi, S, Nah, S, Lee, S-U, Cho, YS, Kim, GW, et al. Cox Regression Model of Prognostic Factors for Delayed Neuropsychiatric Sequelae in Patients with Acute Carbon Monoxide Poisoning: A Prospective Observational Study. Neurotoxicology (2021) 82:63–8. doi:10.1016/j.neuro.2020.11.006
13. Ali-Cherif, A, Royere, ML, Gosset, A, Poncet, M, Salamon, G, and Khalil, R. Behavior and Mental Activity Disorders after Carbon Monoxide Poisoning. Bilateral Pallidal Lesions. Rev Neurol (Paris) (1984) 140(6-7):401–5.
14. Russell, RD, Lucas, RM, Brennan, V, Sherriff, JL, Begley, A, and Black, LJ. Reported Changes in Dietary Behavior Following a First Clinical Diagnosis of Central Nervous System Demyelination. Front Neurol (2018) 9:161. doi:10.3389/fneur.2018.00161
15. Diamond, LM, and Cribbet, MR. Links between Adolescent Sympathetic and Parasympathetic Nervous System Functioning and Interpersonal Behavior over Time. Int J Psychophys (2013) 88(3):339–48. doi:10.1016/j.ijpsycho.2012.08.008
16. Kim, HB, Nah, S, Choi, SW, Kim, GW, Lee, YH, Moon, JE, et al. Objective Predictors of Delayed Neurological Sequelae in Patients with Altered Mental Status after Carbon Monoxide Poisoning. Undersea Hyperb Med (2022) 49(1):83–91.
17. Huang, YQ, Peng, ZR, Huang, FL, and Yang, AL. Mechanism of Delayed Encephalopathy after Acute Carbon Monoxide Poisoning. Neural Regen Res (2020) 15(12):2286–95. doi:10.4103/1673-5374.284995
18. Nock, MK, and Kazdin, AE. Examination of Affective, Cognitive, and Behavioral Factors and Suicide-Related Outcomes in Children and Young Adolescents. J Clin Child Adolesc Psychol (2002) 31:48–58. doi:10.1207/s15374424jccp3101_07
19. Shelef, L, Fruchter, E, Mann, JJ, and Yacobi, A. Correlations between Interpersonal and Cognitive Difficulties: Relationship to Suicidal Ideation in Military Suicide Attempters. Eur Psychiatr (2014) 29(8):498–502. doi:10.1016/j.eurpsy.2014.01.006
20. Yang, K-C, Wang, S-J, Hsieh, W-C, Lirng, J-F, Yang, C-C, Deng, J-F, et al. Longitudinal Changes in the Dopamine Transporter and Cognition in Suicide Attempters with Charcoal Burning. Psychiatry Res Neuroimaging (2015) 231(2):160–7. doi:10.1016/j.pscychresns.2014.12.002
21. Yarlagadda, A, Rosenblatt, KP, and Clayton, AH. Single Nucleotide Polymorphisms and the Central Nervous System: Potential Biomarkers in Identifying Suicide Risk. Innov Clin Neurosci (2017) 14(5-6):21–4.
22. Baca-Garcia, E, Vaquero-Lorenzo, C, Perez-Rodriguez, MM, Gratacòs, M, Bayés, M, Santiago-Mozos, R, et al. Nucleotide Variation in central Nervous System Genes Among Male Suicide Attempters. Am J Med Genet B Neuropsychiatr Genet (2010) 153B(1):208–13. doi:10.1002/ajmg.b.30975
23. Vacchiano, G, and Torino, R. Carbon-monoxide Poisoning, Behavioural Changes and Suicide: An Unusual Industrial Accident. J Clin Forensic Med (2001) 8(2):86–92. doi:10.1054/jcfm.2001.0479
24. Mutluoglu, M, Senol, MG, Yildiz, S, Aydinoz, S, Ay, H, and Uzun, G. Affective Disorder and Suicide Attempt in a Child after Carbon Monoxide Poisoning: Close Follow-Up is Imperative. Pediatr Emerg Care (2011) 27(5):451. doi:10.1097/PEC.0b013e3182187562
25. De Leo, D, Cerin, E, Spathonis, K, and Burgis, S. Lifetime Risk of Suicide Ideation and Attempts in an Australian Community: Prevalence, Suicidal Process, and Help-Seeking Behaviour. J Affect Disord (2005) 86(2-3):215–24. doi:10.1016/j.jad.2005.02.001
26. Ma, X, Xiang, Y-T, Cai, Z-J, Li, S-R, Xiang, Y-Q, Guo, H-L, et al. Lifetime Prevalence of Suicidal Ideation, Suicide Plans and Attempts in Rural and Urban Regions of Beijing, China. Aust N Z J Psychiatry (2009) 43(2):158–66. doi:10.1080/00048670802607170
28. Kessler, RC, Berglund, P, Borges, G, Nock, M, and Wang, PS. Trends in Suicide Ideation, Plans, Gestures, and Attempts in the United States, 1990-1992 to 2001-2003. JAMA (2005) 293(20):2487–95. doi:10.1001/jama.293.20.2487
29. Sun, L, Zhou, C, Xu, L, Li, S, Kong, F, and Chu, J. Suicidal Ideation, Plans and Attempts Among Medical College Students in china: The Effect of Their Parental Characteristics. Psychiatry Res (2017) 247:139–43. doi:10.1016/j.psychres.2016.11.024
30. Bertolote, JM, Fleischmann, A, De Leo, D, Bolhari, J, Botega, N, De Silva, D, et al. Suicide Attempts, Plans, and Ideation in Culturally Diverse Sites: The WHO SUPRE-MISS Community Survey. Psychol Med (2005) 35(10):1457–65. doi:10.1017/s0033291705005404
31. Weaver, LK. Carbon Monoxide Poisoning. Undersea Hyperb Med (2020) 47(1):151–69. doi:10.22462/01.03.2020.17
32. Jia, C-X, Wang, L-L, Xu, A-Q, Dai, A-Y, and Qin, P. Physical Illness and Suicide Risk in Rural Residents of Contemporary china. Crisis (2014) 35(5):330–7. doi:10.1027/0227-5910/a000271
33. Quan, H, Arboleda-Flórez, J, Fick, GH, Stuart, HL, and Love, EJ. Association between Physical Illness and Suicide Among the Elderly. Soc Psychiatry Psychiatr Epidemiol (2002) 37(4):190–7. doi:10.1007/s001270200014
34. Zhang, J, and Sun, L. Suicide Ideation and Acceptability Among Females Aged 15 to 34 Years in Rural China. J Nervous Ment Dis (2014) 202(2):161–6. doi:10.1097/nmd.0000000000000104
35. Casey, P, Dunn, G, Kelly, BD, Lehtinen, V, Dalgard, OS, Dowrick, C, et al. The Prevalence of Suicidal Ideation in the General Population: Results from the Outcome of Depression International Network (ODIN) Study. Soc Psychiat Epidemiol (2008) 43(4):299–304. doi:10.1007/s00127-008-0313-5
36. Cao, X-L, Zhong, B-L, Xiang, Y-T, Ungvari, GS, Lai, KY, Chiu, HF, et al. Prevalence of Suicidal Ideation and Suicide Attempts in the General Population of China: A Meta-Analysis. Int J Psychiatry Med (2015) 49(4):296–308. doi:10.1177/0091217415589306
37. Malakouti, SK, Nojomi, M, Bolhari, J, Hakimshooshtari, M, Poshtmashhadi, M, and De Leo, D. Prevalence of Suicide Thoughts, Plans and Attempts in a Community Sample from Karaj, Iran. Community Ment Health J (2009) 45(1):37–41. doi:10.1007/s10597-008-9173-4
38. Bromet, EJ, Havenaar, JM, Tintle, N, Kostyuchenko, S, Kotov, R, and Gluzman, S. Suicide Ideation, Plans and Attempts in Ukraine: Findings from the Ukraine World Mental Health Survey. Psychol Med (2007) 37(6):807–19. doi:10.1017/s0033291707009981
39. Nock, MK, Borges, G, Bromet, EJ, Alonso, J, Angermeyer, M, Beautrais, A, et al. Cross-national Prevalence and Risk Factors for Suicidal Ideation, Plans and Attempts. Br J Psychiatry (2008) 192(2):98–105. doi:10.1192/bjp.bp.107.040113
40. Lee, S, Fung, SC, Tsang, A, Liu, ZR, Huang, YQ, He, YL, et al. Lifetime Prevalence of Suicide Ideation, Plan, and Attempt in Metropolitan China. Acta Psychiatr Scand (2007) 116(6):429–37. doi:10.1111/j.1600-0447.2007.01064.x
41. Simon, M, Chang, E-S, Zeng, P, and Dong, X. Prevalence of Suicidal Ideation, Attempts, and Completed Suicide Rate in Chinese Aging Populations: A Systematic Review. Arch Gerontol Geriatr (2013) 57(3):250–6. doi:10.1016/j.archger.2013.05.006
42. Clough, BA, March, S, Leane, S, and Ireland, MJ. What Prevents Doctors from Seeking Help for Stress and Burnout? A Mixed-Methods Investigation Among Metropolitan and Regional-Based Australian Doctors. J Clin Psychol (2019) 75(3):418–32. doi:10.1002/jclp.22707
43. Muñoz-Laboy, M, Ripkin, A, Garcia, J, and Severson, N. Family and Work Influences on Stress, Anxiety and Depression Among Bisexual Latino Men in the New York City Metropolitan Area. J Immigrant Minor Health (2015) 17(6):1615–26. doi:10.1007/s10903-015-0220-2
44. Tohmiya, N, Tadaka, E, and Arimoto, A. Cross-sectional Study of Cognitive Stress Appraisal and Related Factors Among Workers in Metropolitan Areas of Japan. BMJ Open (2018) 8(6):e019404. doi:10.1136/bmjopen-2017-019404
45. Wang, C-W, Chan, CLW, and Yip, PSF. Suicide Rates in China from 2002 to 2011: An Update. Soc Psychiatry Psychiatr Epidemiol (2014) 49(6):929–41. doi:10.1007/s00127-013-0789-5
46. Qin, P, and Mortensen, PB. Specific Characteristics of Suicide in China. Acta Psychiatrica Scand (2001) 103(2):117–21. doi:10.1034/j.1600-0447.2001.00008.x
48. Zhang, J, Stewart, R, Phillips, M, Shi, Q, and Prince, M. Pesticide Exposure and Suicidal Ideation in Rural Communities in Zhejiang Province, China. Bull World Health Organ (2009) 87(10):745–53. doi:10.2471/blt.08.054122
49. Zhu, J, Xu, L, Sun, L, Li, J, Qin, W, Ding, G, et al. Chronic Disease, Disability, Psychological Distress and Suicide Ideation Among Rural Elderly: Results from a Population Survey in Shandong. Int J Environ Res Public Health (2018) 15(8):1604. doi:10.3390/ijerph15081604
50. King, CD, Joyce, VW, Nash, CC, Buonopane, RJ, Black, JM, Zuromski, KL, et al. Fear of Sleep and Sleep Quality Mediate the Relationship between Trauma Exposure and Suicide Attempt in Adolescents. J Psychiatr Res (2021) 135:243–7. doi:10.1016/j.jpsychires.2021.01.026
51. Jia, C-X, and Zhang, J. Characteristics of Young Suicides by Violent Methods in Rural China. J Forensic Sci (2011) 56(3):674–8. doi:10.1111/j.1556-4029.2010.01695.x
Keywords: China, population-based study, carbon monoxide poisoning, suicidal ideation, suicide plan
Citation: Sun L, Li K, Zhang Y and Zhang L (2022) Carbon Monoxide Poisoning was Associated With Lifetime Suicidal Ideation: Evidence From A Population-Based Cross-Sectional Study in Hebei Province, China. Int J Public Health 67:1604462. doi: 10.3389/ijph.2022.1604462
Received: 11 September 2021; Accepted: 24 May 2022;
Published: 15 June 2022.
Edited by:
Nino Kuenzli, Swiss Tropical and Public Health Institute (Swiss TPH), SwitzerlandCopyright © 2022 Sun, Li, Zhang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yunshu Zhang, eXVuc2h1Y29mZmVlQHNpbmEuY29t
 Long Sun
Long Sun Keqing Li3
Keqing Li3