- 1Department of Human Geography and Spatial Planning, Faculty of Geosciences, Utrecht University, Utrecht, Netherlands
- 2Department of Interdisciplinary Social Science, Faculty of Social and Behavioural Sciences, Utrecht University, Utrecht, Netherlands
- 3Sciensano, Brussels, Belgium
- 4Chair Group Consumption and Healthy Lifestyles, Wageningen University & Research, Wageningen, Netherlands
Objectives: Government policies are essential to create food environments that support healthy diets. The aims of this study were 1) to benchmark the implementation of Dutch government policies influencing food environments, and 2) to identify and prioritize actions to improve food environments in the Netherlands.
Methods: The Healthy Food Environment Policy Index (Food-EPI) was applied. The Food-EPI includes 46 indicators of food environment policy and infrastructure support. Independent experts (n = 28) rated the extent of implementation on these indicators against international best practices, and formulated and prioritized policy and infrastructure support actions to improve food environments.
Results: Most policy indicators were rated as having a low (50%) or very low (41%) level of implementation. Most infrastructure support indicators were rated as having a fair (42%) or medium (42%) level of implementation. 18 policy and 11 infrastructure support actions were recommended by experts to improve food environments in the Netherlands.
Conclusion: There is large potential for the Dutch national government to strengthen its policy action and infrastructure support in order to improve the healthiness of food environments in the Netherlands.
Introduction
Overweight, obesity and diet-related chronic diseases are a major public health challenge globally [1, 2]. In the Netherlands, approximately 50% of the adult population is overweight [3, 4]. An unhealthy diet is an important determinant of overweight, obesity and diet-related chronic diseases [5, 6]. Unhealthy diets are not merely the result of individual decisions, but strongly influenced by the food environment [7–9].
The food environment can be defined as the physical (e.g., food availability, marketing), economic (food prices), policy and sociocultural surroundings, opportunities and conditions that influence people’s food choices and nutritional status [9]. Over the past few decades, the availability and marketing of ultra-processed, high-fat and sugar-rich products increased, and prices of these products have decreased relatively to healthier foods [8–10]. As commercial interests have been allowed to prevail over public health, this has resulted in so-called obesogenic environments, in which unhealthy food choices are easier made than healthy food choices [8, 11–13].
To correct for this market failure, it is essential that governments develop policies to reverse the obesogenic nature of food environments [8, 11, 14]. Structural, government policies can play an important role to create healthy food environments, supporting the entire population to make healthy food choices [14–17]. These policies are known to be more effective in improving population diets than interventions which address individual behaviour (e.g., health mass media campaigns) [8, 18]. Globally, the implementation of policies to create supportive food environments is low [8, 19]. However, some governments are making progress, for example the Chilean government which implemented a Law of Food Labelling and Advertising, to introduce easy-to-understand front-of-pack labelling and specific messages addressing critical nutrients and to restrict unhealthy food marketing to children across media [20, 21].
In the Netherlands, Article 22 of the Dutch Constitution states that the government should take measures to promote public health [22]. The Dutch government has indeed implemented several voluntary measures to create healthy food environments. For instance, in 2014, the Dutch government signed an Agreement on Product Improvement with the food industry to reduce the amounts of salt, saturated fat and added sugar in products [23]. More recently, in 2018, the Dutch government signed the “National Prevention Agreement” (NPA) together with more than seventy public and private organizations [24, 25]. The NPA specifies goals to reduce overweight among adults from 48.7% in 2017 to 38% in 2040, and among children and adolescents from 13.5% in 2017 to 9.1% in 2040. In addition, the NPA aims to reduce obesity among adults from 14.5% in 2017 to 7.1% in 2040, and among children and adolescents from 2.8% in 2017 to 2.3% in 2040 [24, 25]. To achieve these goals, several voluntary actions have been described in the NPA, e.g., supermarkets will encourage consumers to buy products that are in line with Dutch dietary guidelines (Wheel of Five); the government will introduce a new, broadly supported food-choice logo; and a restriction on the use of licensed media characters aimed at children under 13 years of age on product packaging and point-of-sale materials will be included in the self-regulated Advertising Code for Food [24, 25]. While these voluntary actions can be supportive of healthy food environments, there is lack of structural policies in the NPA (such as the highly contested sugar-sweetened beverages tax, still not implemented in the Netherlands [26]). Contrary to these NPA actions, the Dutch government increased the value-added tax on all foods, including fruits and vegetables, from 6 to 9% in 2019 [27].
Although some actions regarding the improvement of food environments can be observed, a clear and comprehensive picture and evaluation of the current food environment policy landscape in the Netherlands is lacking. To gain more insight into where the largest policy implementation gaps lie and how the Dutch national government could improve its food environment policies, this study applied the Healthy Food Environment Policy Index (Food-EPI) developed by the International Network for Food and Obesity/non-communicable diseases Research, Monitoring and Action Support (INFORMAS) [14]. In applying the Food-EPI tool, this study aims:
1) To benchmark, against international best practices, the extent to which the Dutch national government has implemented policies contributing to a healthy food environment, as well as infrastructure support that facilitates effective policy development and implementation, and
2) To identify and prioritize context-specific actions that can improve food environments in the Netherlands.
Methods
Study Design
This mixed-methods study is conducted as part of the Policy Evaluation Network (PEN) (https://www.jpi-pen.eu/), and under the umbrella of INFORMAS (informas.org). Over the period 2019–2020, we adapted and applied the Food-EPI in the Netherlands [14]. Globally, the Food-EPI has already been applied in more than thirty countries [28]. All procedures performed were in accordance with the ethical standards of the institutional committee [Science-Geosciences Ethics Review Board (SG-ERB), Utrecht University, Netherlands (ERB Review Geo L-19254)] and the Helsinki declaration. All study participants signed informed consent before participation.
Study Procedure
The Food-EPI is an international standardized tool and process to identify important gaps in policies and infrastructure support, and to identify and prioritize future actions to improve food environments [14]. The tool comprises indicators across seven food environment policy domains (food composition, labelling, promotion, prices, provision, retail, trade, and investment) and six infrastructure support domains (leadership, governance, monitoring and intelligence, funding and resources, platforms for interaction, health-in-all-policies) [14]. This study consisted of six steps (see Supplementary Material S1 for an overview of the steps and timeline), which are further outlined below.
Step 1: Tool Adaptation (February–May 2019)
Before applying the Food-EPI to the European context, PEN researchers consulted other researchers/experts to review the 47 original Food-EPI indicators. For each indicator, it was assessed whether the jurisdiction lies with the European Union, national governments or both. Furthermore, PEN researchers asked the participating researchers/experts to indicate whether indicators were clear, needed to be (dis)aggregated or whether indicators were missing. In the food promotion domain one indicator was disaggregated (into restricting promotion through online and social media and promotion in “non-broadcast” media) and one indicator was added (restricting promotion on food packages). In the food provision domain one indicator on public procurement standards in public sector settings was added. It was decided to include the trade domain (including two indicators) in the EU Food-EPI, but not in the national Food-EPI’s. This resulted in a total of 46 indicators included in the Dutch Food-EPI, i.e., 22 policy and 24 infrastructure support indicators (Supplementary Material S2).
Steps 2–3: “Evidence Document” and Online Benchmarking Survey
In step 2, evidence for the implementation of policies for each of the 46 Food-EPI indicators (up until 22 April 2020) in the Netherlands was collected through systematically searching for and reading national policy documents. We used several main sources to search for the relevant policy documents, including the national government websites (e.g., https://wetten.overheid.nl, htttps://www.rivm.nl, https://www.voedingscentrum.nl, https://www.rijksoverheid.nl). Via these websites we found information and links to additional useful documents including the Agreement on Product Improvement, the NPA, and the Advertising Code for Food. All policies identified at the national level with a potential influence on the food environment have been summarized in an 34-page “evidence document” [29]. This document was verified for completeness and accuracy by governmental officials, for example by officials working at the Ministry of Health, Netherlands Nutrition Centre and the National Institute for Public Health and the Environment.
After a brainstorm with the research team we developed a long list of relevant Dutch organizations in the field of food and nutrition, public health, obesity, and/or diet-related chronic diseases, i.e., academia, health organizations, health professional associations, non-governmental organizations, and local governments. Further, we created a long list of names of people working at these organizations, and purposively invited them to participate in the Dutch Food-EPI expert panel (March–May 2020). To ensure that all relevant expertise would be represented in the expert panel, invited experts were asked to supply the research team with any names of other relevant experts that should be invited for the Food-EPI expert panel.
In total 52 independent experts were invited. In step 3, they were asked to benchmark the implementation of policies and infrastructure support against international best practices during an online survey. A total of 28 experts filled out the survey (May–July 2020), of which 25 experts fully completed and 3 partly. Participants benchmarked the implementation of each of the 22 policy and 24 infrastructure support indicators, by comparing the level of implementation as described in the evidence document to international best practices (i.e., comprehensive examples of policy implementation worldwide which were provided for each indicator). The guidance that was given to the experts to determine the level of implementation has been included in Supplementary Material S3. A five-point Likert scale was included to benchmark the implementation of policies, with 1 = 0–20% implementation (=very low), 2 = 20–40% implementation (=low), 3 = 40–60% implementation (=medium), 4 = 60–80% implementation (=fair), and 5 = 80–100% implementation (=high). There was also a ‘cannot rate’ option and experts could comment on their rating in a text box.
Moreover, experts were asked to write down concrete actions (for each policy and infrastructure domain) that they considered important in order to improve the healthiness of food environments in the Netherlands.
Steps 4–6: Identification and Prioritization of Actions to Improve Food Environments in the Netherlands
Due to the 2020 Covid-19 bans on travel and meetings, the next logical step in the Food-EPI process, i.e., a face-to-face workshop with the expert panel to discuss the proposed actions, was not possible. Therefore, a different approach than outlined in the Food-EPI protocol [30] was taken, as described below in step 4–6.
Step 4 Online Workshops
To combine and narrow down (e.g., omit duplications) the actions as proposed by the expert panel (n = 28) during the online benchmarking survey (step 3), two online workshops of 3-hours each were held (September 2020). As there were many (189) actions formulated during the online benchmarking survey which had to be combined and narrowed down, we invited a selected group of experts (n = 4) (who also had completed the online benchmarking survey) to ensure an effective and efficient online discussion. Two of these experts were specialized in public health and nutrition working in health organizations and two of these experts were specialized in nutrition and food law/politics working in academia. For each domain, the experts were also consulted if any important actions were missing on the list.
Step 5a Refining Actions
The research team made final adjustments to the list of actions according to the input received during the workshops. This adjusted list of actions was then sent to the four experts who participated in the online workshops for verification.
Step 5b Online Selection Survey to Investigate Which Actions to Recommend
The expert panel (n = 28) was invited for a second online selection survey in October 2020. They were asked to indicate for each of the actions if they would recommend the Dutch government to implement this action, using a five-point Likert scale: 1) very much disagree 2) disagree 3) neutral 4) agree 5) very much agree. A total of 17 experts participated in this survey.
Step 6 Prioritization of the Recommended Actions
In the third and final online survey (November 2020), the expert panel (n = 28) was asked to prioritize the recommended actions that received an average score of 4.0 or higher in step 5b. A total of 21 experts completed this prioritization survey. Experts ranked the policy actions three times on 1) importance, 2) achievability and 3) equity, i.e., the effect on socioeconomic inequalities in diet. Experts ranked the infrastructure support actions twice on 1) importance and 2) achievability. Importance includes criteria on need, impact, and other positive and negative effects. Achievability includes criteria on feasibility, acceptability, affordability, and efficiency. And equity includes criteria on socioeconomic effects (regressive/progressive) and the extent to which a given policy requires environmental change rather than individual choices. Supplementary Material S4 includes a comprehensive description of the ranking criteria. When an action was ranked as #1 it was considered to be most important, achievable or equitable.
Data Analysis
The mean score on the five point Likert scale was calculated for each indicator to determine the implementation of policies. The Gwet AC2 inter-rater reliability coefficient and its variance were determined using AgreeStat software (Agreestat 2015.6.1, Advanced Analytics, Gaithersburg, United States). For estimation of the variance, the sample of subjects to rate was set at 100% since all indicators of the Food-EPI were included for rating, while the sample of raters was set at 54% (as per the response rate of experts invited), and the finite population correction was applied (step 3).
Regarding step 5b, the mean score was calculated for each action based on the five point Likert scale. Actions with a mean score of 4.0 or higher were included in step 6.
In step 6, we identified the highest prioritized policy and infrastructure actions by summing the ranking scores for each action. First, we calculated the scores for importance and achievability separately. Second, we calculated the total score for each action by summing the scores on importance and achievability. Sum scores could vary from 42 to 756 (policy domains) and from 42 to 462 (infrastructure support domains). A lower sum score indicated a higher perceived priority. These sum scores were used to determine the top 5 prioritized policy actions and the top 5 prioritized infrastructure support actions. For the policy actions, we also calculated the sum of the scores on equity for each action and determined the top 5 actions which were perceived most effective to reduce socioeconomic inequalities in diet.
Results
Expert Panel
The 28 experts that participated in this study were working in academia, health organizations/health professional associations, non-governmental organizations (NGO’s) and local governments, and specialised in food, nutrition, public health, obesity and/or diet-related chronic diseases (Supplementary Material S5). In the online benchmarking survey participation was highest (12 experts from academia, six from health organizations/health professional associations, four from NGO’s and six from local governments), followed by the prioritisation survey (10 experts from academia, five from health organizations/health professional associations, three from NGO’s and three from local governments). The least experts participated in the selection survey (eight from academia, five from health organizations/health professional associations, three from NGO’s and one from a local government).
Ratings of the Extent of Implementation of Policies and Infrastructure Support Influencing Food Environments Compared to Best Practice
Figures 1 and 2 present for each Food-EPI indicator separately, the mean implementation score of policies and infrastructure support in the Netherlands compared to international best practices, according to the experts. The Inter-rater reliability (Gwet’s AC2) for all Food-EPI indicators was 0.57 (95% CI = 0.51–0.62), which indicates that there was moderate agreement among experts about the implementation of policies against international best practices. There was strong agreement about the policy indicators (Gwet’s AC2 was 0.78; 95% CI = 0.73–0.83), but lower agreement about the infrastructure support indicators (Gwet’s AC2 was 0.46; 95% CI = 0.39–0.53).
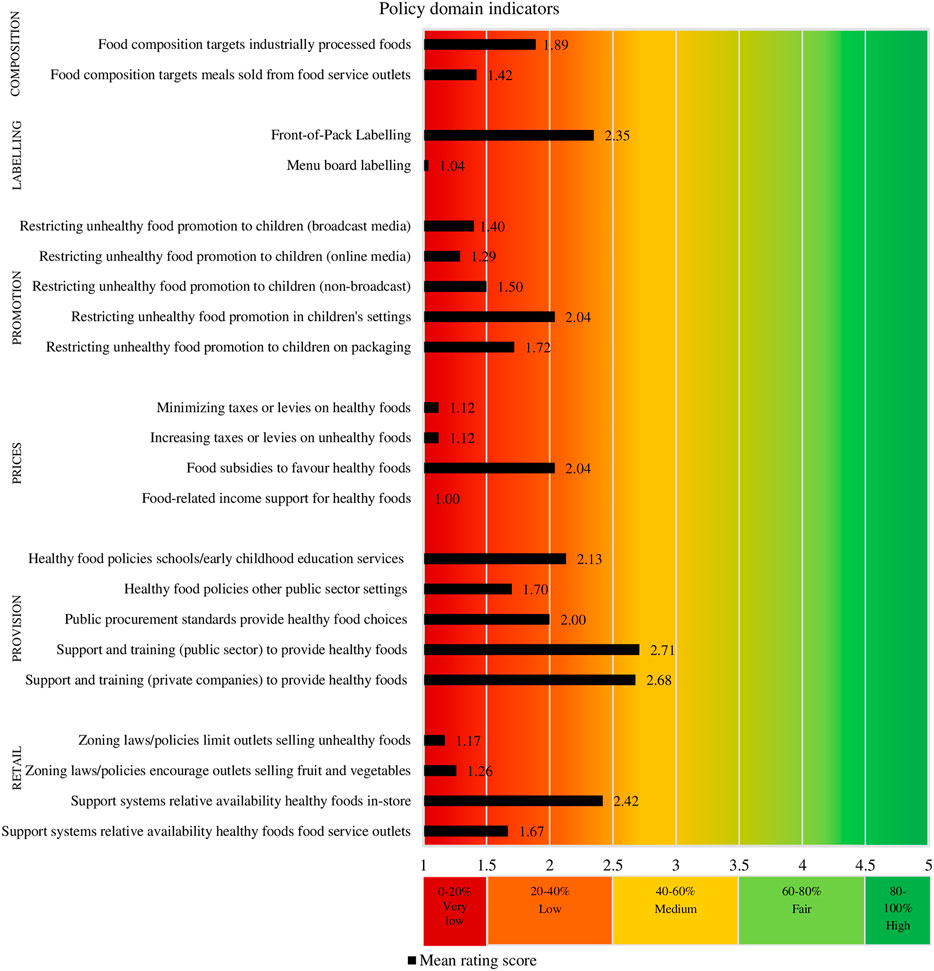
FIGURE 1. Ratings of the extent of implementation of policies influencing food environments. (Food-EPI study, the Netherlands, 2019–2020).
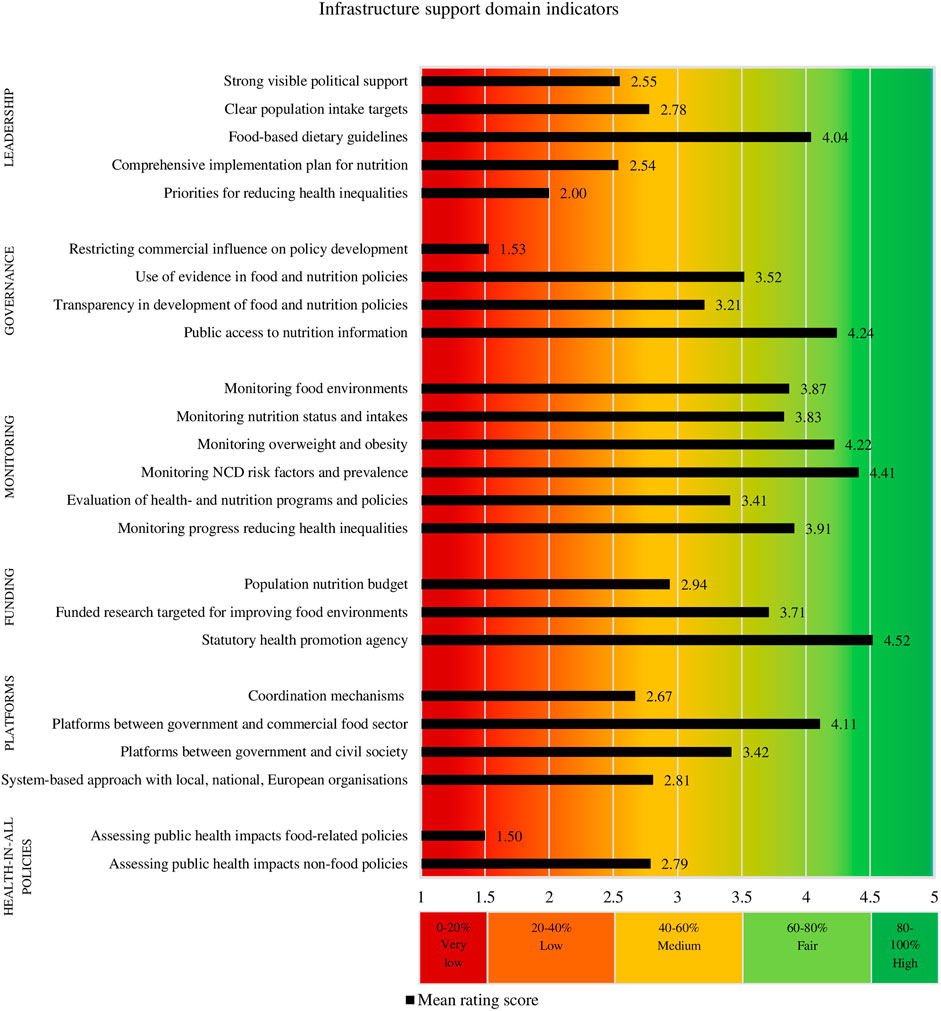
FIGURE 2. Ratings of the extent of implementation of infrastructure support influencing food environments. (Food-EPI study, the Netherlands, 2019–2020).
Policy Domains
The implementation of 50% of the indicators in the policy domains (11 of the 22 indicators) was rated as being “low” (20–40% implementation) (Figure 1). Yet, the implementation of 41% of the policies (nine of the 22 indicators) was rated even being “very low” (0–20% implementation). The expert panel considered the implementation of policies with respect to two of the 22 (9%) policy indicators as being “medium” (40–60% implementation).
Infrastructure Support Domains
The implementation of infrastructure support indicators was generally rated higher than policy indicators (Figure 2). The implementation of one of the 24 infrastructure support indicators, namely “having a statutory health promotion agency in place” (Funding domain) was rated “high” by the expert panel. This includes the Netherlands Nutrition Centre and the National Institute for Public Health and the Environment.
Further, the implementation of 10 of the 24 infrastructure support indicators (42%) was rated being “fair,” another 10 (42%) as being “medium,” and three indicators (12%) were rated as having “low” implementation compared to international best practices (Figure 2). In contrast to the policy indicators, no infrastructure support indicators were rated as having “very low” implementation.
Identification and Prioritization of Actions to Improve Policies and Infrastructure Support
Based on step 3 (benchmark survey), step 4 (workshops) and step 5a (refinements), a total of 46 actions were proposed by the expert panel, namely 27 policy actions and 19 infrastructure support actions. In step 5b (selection survey), a total of 29 actions, including 18 policy actions and 11 infrastructure support actions were scored with a 4.0 or higher and thereby recommended to the national government to create healthy food environments in the Netherlands.
Recommended and Prioritized Policy Actions
The 18 policy actions recommended by the experts are detailed in Table 1. The actions are listed in order of priority considering both importance and achievability. The five actions with the highest potential to reduce dietary socioeconomic inequalities according to the experts are marked with an asterisk (*).
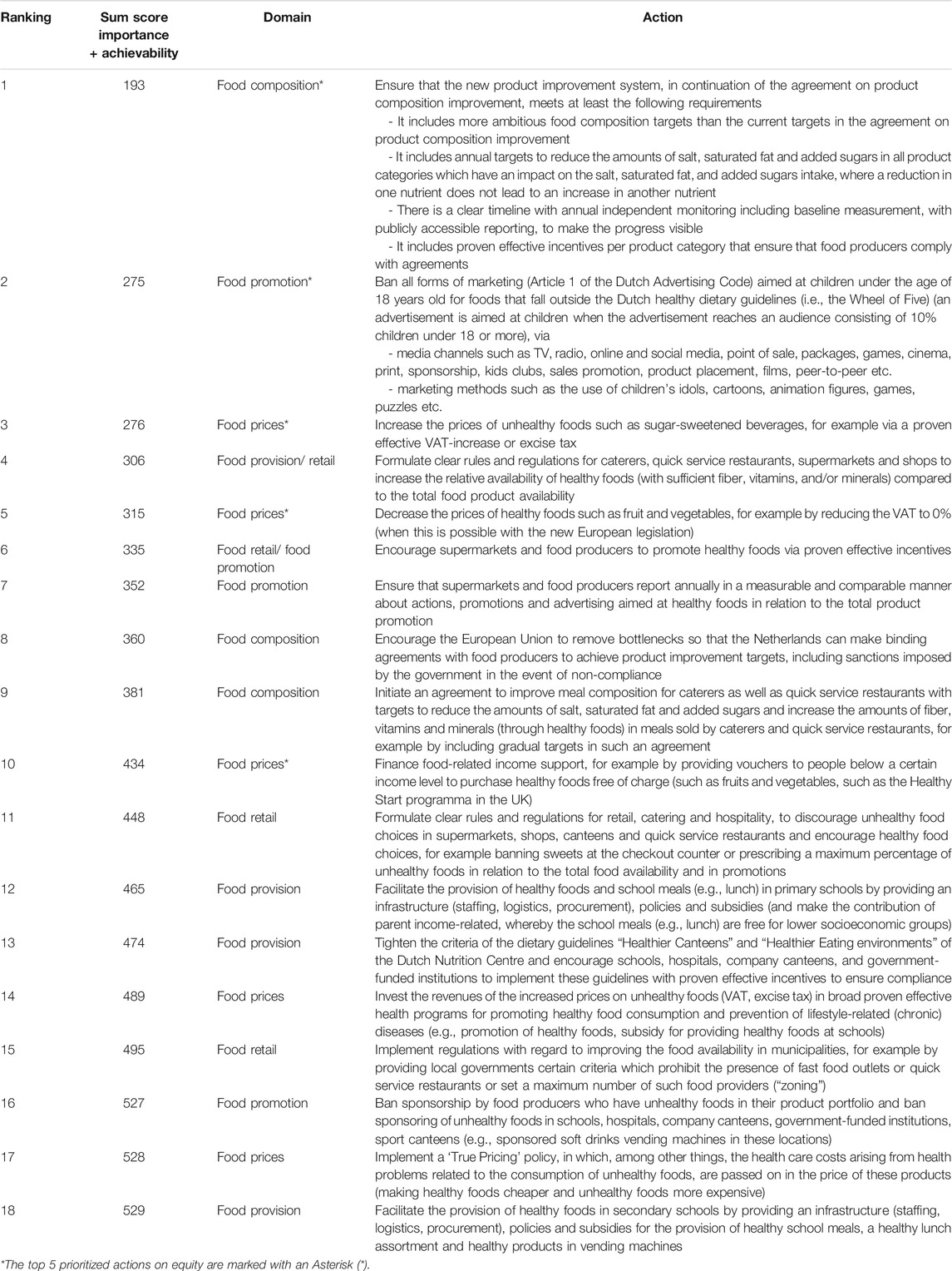
TABLE 1. Policy actions to create healthy food environments, recommended by the Food-EPI expert Panel (listed in order of prioritization on a combination of importance and achievability). (Food-EPI study, the Netherlands, 2019–2020).
Four of the top 5 prioritized policy actions on importance and achievability, also appeared in the top 5 actions with the greatest potential to reduce dietary socioeconomic inequalities. These four actions, together with the other top 5 action on importance and achievability, and the other top 5 action on equity (six in total) were recommended to the government for immediate implementation.
In Figure 3, the scores on importance and achievability for each action are plotted in a graph, and the five actions with the greatest potential to reduce socioeconomic inequalities in diet are indicated by a yellow shadow.
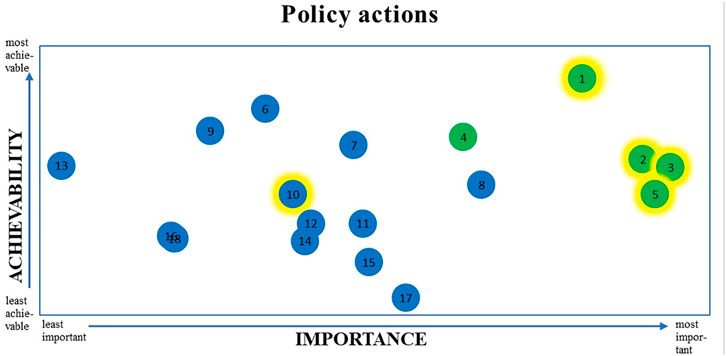
FIGURE 3. Importance and achievability of recommended policy actions for the Dutch national government and the top 5 actions which have the greatest potential to reduce socioeconomic inequalities in diet*. *The top 5 priority policy actions on a combination of importance and achievability are shown in green; the five actions which have the greatest potential to reduce socioeconomic inequalities in diet are indicated by the yellow shadow. See Table 1 for a description of the 18 policy actions. (Food-EPI study, the Netherlands, 2019–2020).
Recommended and Prioritized Infrastructure Support Actions
The 11 infrastructure support actions recommended by the Food-EPI expert panel are detailed in Table 2. The actions are listed in order of priority considering both importance and achievability. The top 5 prioritized actions were recommended to the government for immediate implementation. Each infrastructure support action is plotted on importance and achievability in Figure 4.
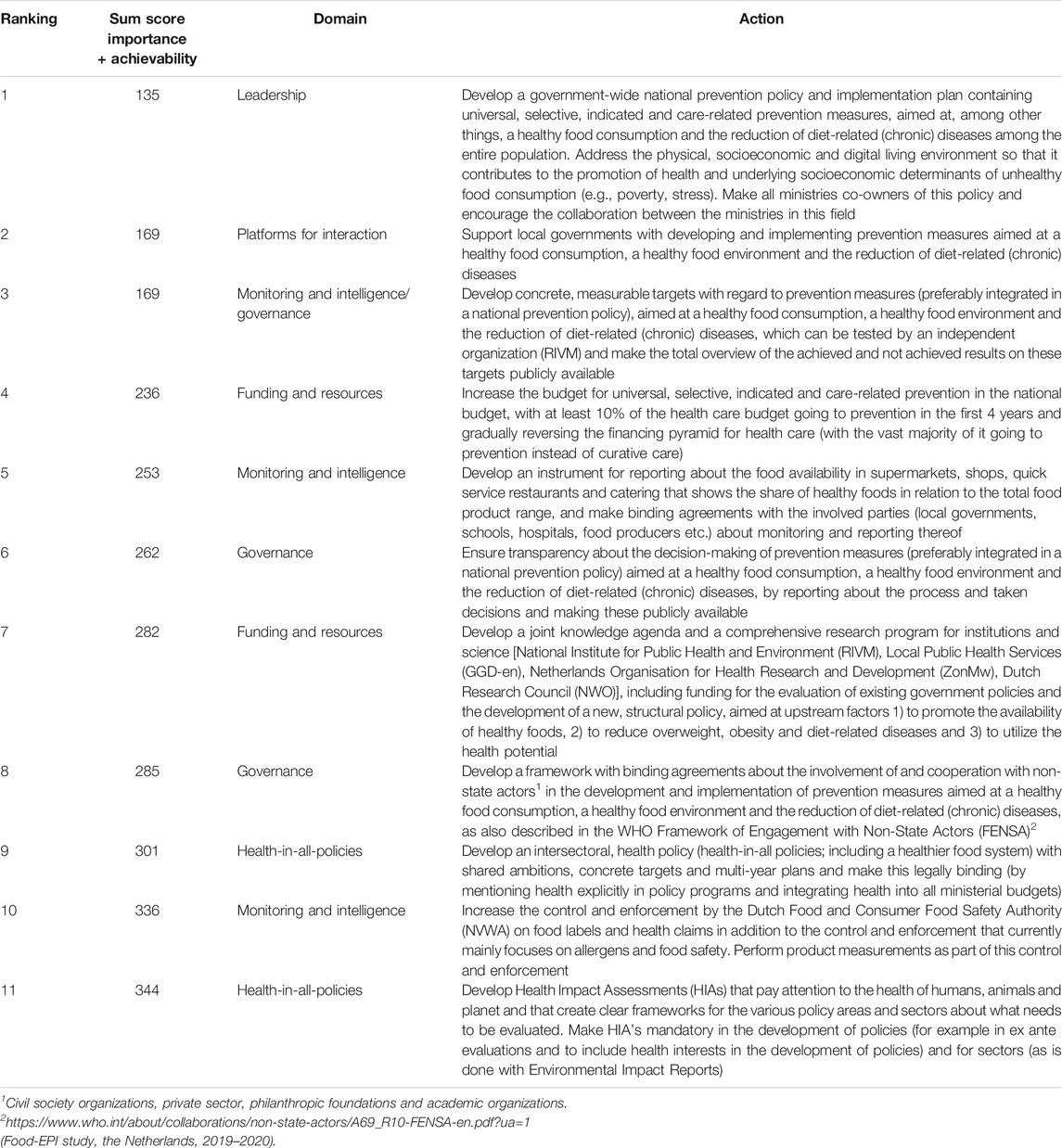
TABLE 2. Infrastructure support actions, recommended by the Food-EPI expert panel (listed in order of prioritization on a combination of importance and achievability).
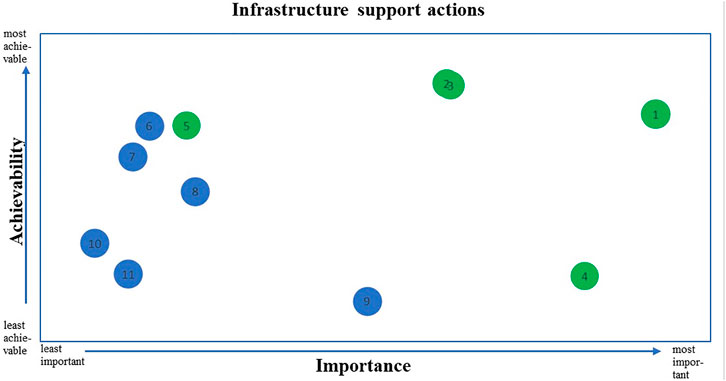
FIGURE 4. Importance and achievability of recommended infrastructure support actions for the Dutch national government*. *The top 5 priority infrastructure support actions on a combination of importance and achievability are shown in green. See Table 2 for a description of the 11 infrastructure support actions. (Food-EPI study, the Netherlands, 2019–2020).
Discussion
This study showed that there are several gaps in the implementation of food environment policies and infrastructure support in the Netherlands. Moreover, results indicate that there are relatively more implementation gaps with regard to policies directly influencing food environments (policy domains) than with regard to infrastructure support facilitating the development and implementation of policies (infrastructure support domains). A total of 18 policy and 11 infrastructure support actions to create healthier food environments in the Netherlands have been identified that can be implemented by the Dutch government.
The outcomes of this Food-EPI study for the Netherlands were in line with international observations. An 11-country Food-EPI comparison study showed that the implementation of infrastructure support was rated higher than the implementation of food environment policies in all countries, except Chile [20]. Also in Ireland and Norway, where comparable Food-EPI studies were conducted as part of the Policy Evaluation Network, the implementation of infrastructure support was rated higher than the implementation of the policy indicators [31, 32].
There are a number of possible explanations for the low implementation of policies directly influencing food environments. First, the food industry has a diverse range of strategies to influence governmental policies, such as lobbying, participation in meetings with governments, and promoting industry-preferred solutions such as education and voluntary initiatives which rely on self-regulation, rather than mandatory governmental regulations [12, 33–37]. Second, the influence of these strategies is strengthened by a lack of political will to implement structural, universal, obesity and diet-related chronic diseases prevention measures [37]. The WHO indicated that not one single country has managed to turn around the obesity epidemic, because of a failure of political will to take on big business [38]. Like the default in many countries [39], voluntary self-regulation is the common approach to improve food availability and promotion in the Netherlands. The past governing coalitions consisted of mainly liberal and confessional parties where self-regulation by the industry has been an important tradition in health policy development and implementation [40]. To illustrate, in 2014, the Minister of Health came to a national agreement with representatives of the food industry to improve product composition [23, 41]. Businesses concluded voluntary chain agreements to reduce the content of salt, saturated fat and added sugar in their products [42]. There were no incentives from the government if the industry would not meet these agreements [23]. More recently (2018), as part of the NPA, the national government installed a committee with 70 organizations that represented a wide variety of stakeholders including associations of health charities, municipalities, primary and secondary education, municipal health services, health professionals, health care insurance companies, but also associations of the food industry, supermarkets, catering companies, and restaurants [43]. As part of this committee agreements to reduce overweight prevalence in the Netherlands where brokered [43]. This led to an NPA only containing voluntary measures to create healthy food environments [24, 25]. According to the National Institute for Public Health and the Environment, with the agreements to improve product composition only small steps are taken [44–46] and the measures in the NPA will only lead to a limited slowdown in the increase in overweight and obesity [47]. Indeed, according to literature, improvements of the food environment as a result of voluntary self-regulated approaches by the industry are mostly weak and there is little evidence of their effectiveness in improving population diets and preventing obesity and diet-related chronic diseases [39, 48].
As appears from the recommended and prioritized actions in our study, there is a need for less self-regulation and more ambitious, structural, universal interventions by the Dutch government. This need has also been recognized by the State Secretary for Health in a reaction to our Food-EPI report [49]. In the recently published coalition agreement 2021–2025, the new Dutch government announces a few structural and strict measures towards healthier food environments [50]. Actions included in this agreement are making binding agreements with the food industry about healthier foods, increasing taxes on sugar-sweetened beverages and investigating how to introduce a sugar tax and lower the current VAT tariff of 9% on vegetables and fruit to 0% [50]. Furthermore, the government promises to protect children against inappropriate online promotion and marketing [50]. However, it is not specified if this will also include protection against food marketing, which is currently regulated via the Advertising Code for Food products (2019) [51] initiated by the Dutch Food Industry Federation [52, 53].
Like the Netherlands, most European countries currently also have mainly voluntary initiatives [54], but some have already implemented more extensive measures. For example, regarding restricting unhealthy food marketing to children, the UK is considering a total ban on online advertising of foods high in fat, sugar, or salt to children [55]. In Portugal, Law 30/2019 restricts unhealthy food advertising directed to children via broad-cast media and digital marketing [56].
Related to price measures, various other European countries have already implemented food-related health taxes, such as the sugar-sweetened beverages taxes in the UK, Ireland, France, Spain, Portugal and the public health product tax in Hungary [57]. Also, several European countries apply a lower VAT-tariff on fruits and vegetables than the 9% in the Netherlands, such as the UK and Ireland (0%), Spain and Italy (4%) and Poland and Latvia (5%) [58]. Such structural policies more likely result in sustainable food consumption changes of the whole population including vulnerable groups, which could contribute to a reduction in socioeconomic inequalities in diet [8, 59, 60]. As the impact of combined interventions is greater than the impact of single interventions, experts in this study emphasized that measures should be part of a comprehensive, population-wide approach to prevent obesity and diet-related chronic diseases [61, 62].
Differently than in other Food-EPI studies, in the PEN Food-EPI’s experts were also asked to prioritize the policy actions on equity. Experts in our study indicated that price actions have the greatest potential to reduce socioeconomic inequalities in diet, which was also shown by an umbrella and systematic review [63, 64]. However, experts also indicated that food composition and marketing policies could be pro-equity, for which less empirical evidence was found [63, 64].
For this study we also have to consider that the Dutch national government is dependent on EU regulations. A Food-EPI study at EU-level was conducted to gain insight into the policies that need to be improved to create healthy food environments in EU Member States [65]. Thus, in addition to the actions that the Dutch national government can implement immediately, some actions (e.g., allowing a VAT of 0% on fruits and vegetables which was recently agreed on by the EU finance ministers and on which the European Parliament will be consulted [66]) cannot be implemented without policy changes at EU-level. It is therefore essential that national governments stimulate the EU to remove bottlenecks for creating healthy food environments at national level.
Strengths and Limitations
This study has some important strengths. This is the first study in the Netherlands that applied a comprehensive mixed-methods approach in order to generate insight into the largest policy and infrastructure support implementation gaps as well as government actions to improve food environments. Second, policies described in the evidence document were verified by governmental officials and implementation of policies was evaluated by independent experts.
Nevertheless, some limitations should be acknowledged. First, due to the Covid-19 restrictions on travel and meetings, the workshop (step 4) was conducted online with a small group of experts instead of the envisaged face-to-face meeting with the entire expert panel. In addition, we were experiencing drop-out in participation, as a lower number experts participated in the follow-up surveys (n = 17, n = 21) compared to the first survey (n = 28), which showed the limitations of an online procedure. This might have impacted on the results regarding the recommended actions and ranking of the actions that should be considered. However, the diverse range of expertise of experts that did participate in the follow-up surveys, still make the results representative for the Dutch experts in the field of food, nutrition, public health, obesity, and/or diet-related chronic diseases. Moreover, compared to other international Food-EPI studies, the number of experts that participated in our final online prioritization survey (n = 21) is in line with other countries [31, 32]. Although we used an international standardized framework to assess food environmental policies from a public health perspective, the methodology is susceptible to subjectivity. A final limitation is that the Food-EPI does not identify why policies have or have not been successfully implemented [67]. Identifying the barriers and facilitators to implementing food environment policies could give important additional insights into how the national government could enable the implementation of these policies [68].
We also have some recommendations for future research. This study constructed scorecards (Figures 1, 2) on the implementation of national government policies, which facilitates monitoring of these policies over time, for example every five years. In the long-term, this study can contribute to a global database for monitoring and evaluating food environment policies. Another recommendation is to identify why recommended policies have or have not been successfully implemented, which can support uptake of policies [68]. A final recommendation is to compare the study outcomes, with outcomes of the other Food-EPI studies conducted as part of PEN (EU-level, Ireland, Norway, Poland, Germany) and the H2020 Science and Technology in childhood Obesity Policy (STOP) project (Slovenia, Spain, Portugal, Estonia, Finland).
Conclusion
Experts consider the implementation of Dutch government policies directly influencing food environments largely as very low to low, while the implementation of infrastructure support was rated fair to medium. Recommended actions should be implemented by the Dutch government to create healthier food environments in the Netherlands.
Ethics Statement
The study was conducted according to the ethical standards declared in the 1964 Declaration of Helsinki and its later amendments. This study was granted ethical approval by the Science-Geosciences Ethics Review Board (SG-ERB), Utrecht University, The Netherlands (ERB Review Geo L-19254). The participants provided their written informed consent to participate in this study.
Author Contributions
SV, CK, MP, and SD reviewed and discussed together with other PEN researchers the original Food-EPI indicators to assess if these indicators needed to be adjusted before applying them to the European context. SD collected the evidence for the implementation of policies in the Netherlands. SD in collaboration with CK and MP summarized the evidence in an 34-page “evidence document”. SD, MP, and CK set up a list with experts to invite for the Expert panel. SD sent invitations to the experts. SD, in collaboration with MP and CK set up and conducted the benchmarking, selection and prioritization surveys. SD analyzed the results of these surveys. SD, MP, and CK prepared and conducted the online workshops with a selected group of experts to discuss the actions formulated. SD adjusted the action list according to the input received. SD, together with CK and MP had the lead in writing this manuscript. SV critically reviewed the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that this study received funding from The Netherlands Organization for Health Research and Development (ZonMw), project number 529051020. ZonMw had no role in the design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank all the experts who participated in study for their time, efforts and valuable contributions. This research is part of the Policy Evaluation Network (PEN): https://www.jpi-pen.eu/. PEN is funded by the Joint Programming Initiative: a Healthy Diet for a Healthy Life (JPI-HDHL): https://www.healthydietforhealthylife.eu/, a research and innovation initiative of EU member states and associated countries. The funding agencies supporting this work are (in alphabetical order of participating countries): France: Institut National de la Recherche Agronomique (INRA); Germany: Federal Ministry of Education and Research (BMBF); Ireland: Health Research Board (HRB); Italy: Ministry of Education, University and Research (MIUR); The Netherlands: The Netherlands Organization for Health Research and Development (ZonMw); New Zealand: The University of Auckland, School of Population Health; Norway: The Research Council of Norway (RCN); Poland: The National Centre for Research and Development (NCBR).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2022.1604115/full#supplementary-material
References
1. Ng, M, Fleming, T, Robinson, M, Thomson, B, Graetz, N, Margono, C, et al. Global, Regional, and National Prevalence of Overweight and Obesity in Children and Adults during 1980-2013: A Systematic Analysis for the Global burden of Disease Study 2013. Lancet (2014) 384(9945):766–81. doi:10.1016/S0140-6736(14)60460-8
2.NCD Risk Factor Collaboration (NCD-RisC) Abarca-Gómez, L, Abdeen, ZA, Hamid, ZA, Abu-Rmeileh, NM, Acosta-Cazares, B, Acuin, C, et al. Worldwide Trends in Body-Mass index, Underweight, Overweight, and Obesity from 1975 to 2016: a Pooled Analysis of 2416 Population-Based Measurement Studies in 128·9 Million Children, Adolescents, and Adults. Lancet (2017) 390(10113):2627–42. doi:10.1016/S0140-6736(17)32129-3
3.Rijksinstituut. Cijfers en feiten overgewicht. Rijksinstituut voor Volksgezondheid en Milieu (2021). Available at: https://www.loketgezondleven.nl/gezondheidsthema/overgewicht/cijfers-en-feiten-overgewicht (Accessed March 18, 2021).
4.Rijksoverheid. Cijfers en context. Rijksinstituut voor Volksgezondheid en Milieu (2021). Trend overgewicht volwassenen. https://www.volksgezondheidenzorg.info/onderwerp/overgewicht/cijfers-context/trends#node-trend-overgewicht-volwassenen (Accessed March 18, 2021).
5.World Health Organization. Factsheet Obesity and Overweight (2020). Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (Accessed March 18, 2021).
6. Willett, W, Rockström, J, Loken, B, Springmann, M, Lang, T, Vermeulen, S, et al. Food in the Anthropocene: the EAT-Lancet Commission on Healthy Diets from Sustainable Food Systems. The Lancet (2019) 393(10170):447–92. doi:10.1016/s0140-6736(18)31788-4
7. Vandenbroeck, P, Goossens, J, and Clemens, M. Foresight Tackling Obesities: Future Choices — Obesity System Atlas. UK Government’s Foresight Programme (2007). Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/295153/07-1177-obesity-system-atlas.pdf (Accessed March 18, 2021).
8. Swinburn, BA, Sacks, G, Hall, KD, McPherson, K, Finegood, DT, Moodie, ML, et al. The Global Obesity Pandemic: Shaped by Global Drivers and Local Environments. The Lancet (2011) 378(9793):804–14. doi:10.1016/s0140-6736(11)60813-1
9. Swinburn, B, Sacks, G, Vandevijvere, S, Kumanyika, S, Lobstein, T, Neal, B, et al. INFORMAS (International Network for Food and Obesity/non-Communicable Diseases Research, Monitoring and Action Support): Overview and Key Principles. Obes Rev (2013) 14(S1):1–12. doi:10.1111/obr.12087
10. Poelman, MP, Kamphuis, CBM, and van Lenthe, F. Voedselconsumptie Vanuit Gedragsperspectief (2018). Available at: https://gof.sites.uu.nl/wp-content/uploads/sites/186/2018/04/Voedsel_-Duurzame-en-gezonde-keuzes-voor-consumptie.pdf (Accessed March 18, 2021).
11. Moodie, R, Swinburn, B, Richardson, J, and Somaini, B. Childhood Obesity - a Sign of Commercial success, but a Market Failure. Int J Pediatr Obes (2006) 1(3):133–8. doi:10.1080/17477160600845044
12. Mialon, M. An Overview of the Commercial Determinants of Health. Glob Health (2020) 16(1):74. doi:10.1186/s12992-020-00607-x
13. White, M, Aguirre, E, Finegood, DT, Holmes, C, Sacks, G, and Smith, R. What Role Should the Commercial Food System Play in Promoting Health through Better Diet? BMJ (2020) 368:m545. doi:10.1136/bmj.m545
14. Swinburn, B, Vandevijvere, S, Kraak, V, Sacks, G, Snowdon, W, Hawkes, C, et al. Monitoring and Benchmarking Government Policies and Actions to Improve the Healthiness of Food Environments: a Proposed G Overnment H Ealthy F Ood E Nvironment P Olicy I Ndex. Obes Rev (2013) 14(S1):24–37. doi:10.1111/obr.12073
15. Gorski, MT, and Roberto, CA. Public Health Policies to Encourage Healthy Eating Habits: Recent Perspectives. J Healthc Leadersh (2015) 7:81–90. doi:10.2147/JHL.S69188
16. Mozaffarian, D, Angell, SY, Lang, T, and Rivera, JA. Role of Government Policy in Nutrition-Barriers to and Opportunities for Healthier Eating. BMJ (2018) 361:k2426. doi:10.1136/bmj.k2426
17.World Health Organization. Regional Office for Europe. European Food and Nutrition Action Plan 2015-2020 (2015). Copenhagen, Denmark. Available at: https://www.euro.who.int/__data/assets/pdf_file/0008/253727/64wd14e_FoodNutAP_140426.pdf (Accessed March 18, 2021).
18. Story, M, Kaphingst, KM, Robinson-O'Brien, R, and Glanz, K. Creating Healthy Food and Eating Environments: Policy and Environmental Approaches. Annu Rev Public Health (2008) 29(1):253–72. doi:10.1146/annurev.publhealth.29.020907.090926
19. Roberto, CA, Swinburn, B, Hawkes, C, Huang, TT-K, Costa, SA, Ashe, M, et al. Patchy Progress on Obesity Prevention: Emerging Examples, Entrenched Barriers, and New Thinking. The Lancet (2015) 385(9985):2400–9. doi:10.1016/s0140-6736(14)61744-x
20. Vandevijvere, S, Barquera, S, Caceres, G, Corvalan, C, Karupaiah, T, Kroker‐Lobos, MF, et al. An 11‐country Study to Benchmark the Implementation of Recommended Nutrition Policies by National Governments Using the Healthy Food Environment Policy Index, 2015‐2018. Obes Rev (2019) 20(S2):57–66. doi:10.1111/obr.12819
21. Corvalán, C, Reyes, M, Garmendia, ML, and Uauy, R. Structural Responses to the Obesity and Non-communicable Diseases Epidemic: The Chilean Law of Food Labeling and Advertising. Obes Rev (2013) 14(S2):79–87. doi:10.1111/obr.12099
22.De Nederlandse grondwet. Artikel 22: Volksgezondheid; Woongelegenheid; Ontplooiing (Updated 2005). De Nederlandse grondwet (2021). Available at: https://www.denederlandsegrondwet.nl/id/via0icz1nezn/artikel_22_volksgezondheid (Accessed March 18, 2021).
23. Roetert, B, van den Berg, B, van der Grinten, LJHM, and Verheij, T. Schippers EI (Minister of Health, Welfare and Sport (VWS)). National Agreement to Improve Product Composition 2014-2020 (2014). Available at: https://www.akkoordverbeteringproductsamenstelling.nl/en (Accessed March 18, 2021).
24.National Prevention Agreement. National Government. Ministry of Health, Welfare and Sport. The National Prevention Agreement. A Healthier Netherlands (2019). Available at: https://www.government.nl/documents/reports/2019/06/30/the-national-prevention-agreement (Accessed March 18, 2021).
25.Rijksoverheid. Ministerie van Volksgezondheid, Welzijn en Sport. Nationaal Preventieakkoord (2018). Available at: https://www.rijksoverheid.nl/documenten/convenanten/2018/11/23/nationaal-preventieakkoord (Accessed March 18, 2021).
26.World Health Organization. Taxes on Sugary Drinks (Updated 2019) (2019). Available at: https://www.who.int/southeastasia/news/feature-stories/detail/taxes-on-sugary-drinks (Accessed March 18, 2021).
27.Rijksoverheid. Belangrijkste Belastingwijzigingen Per 1 Januari 2019 (Updated 2018) (2018). Available at: https://www.rijksoverheid.nl/actueel/nieuws/2018/12/18/belangrijkste-belastingwijzigingen-per-1-januari-2019#:∼:text=Het%20kabinet%20betaalt%20de%20verlaging,%E2%82%AC%202%2C83%20duurder%20worden (Accessed March 18, 2021).
28. Sacks, G, Kwon, J, Vandevijvere, S, and Swinburn, B. Benchmarking as a Public Health Strategy for Creating Healthy Food Environments: An Evaluation of the INFORMAS Initiative (2012-2020). Annu Rev Public Health (2021) 42:345–62. doi:10.1146/annurev-publhealth-100919-114442
29. Djojosoeparto, SK, Kamphuis, CBM, and Poelman, MP. The Healthy Food Environment Policy index (Food-EPI): Nederland. Evidence Document Summarizing National Governmental Policies Affecting the Food Environment in the Netherlands. Netherlands: Utrecht University (2020) (Accessed March 18, 2021).
30. Vandevijvere, S. INFORMAS PROTOCOL PUBLIC SECTOR MODULE. Healthy Food Environment Policy Index (Food-EPI) (2017). Available at: https://figshare.com/articles/journal_contribution/INFORMAS_Protocol_Public_Sector_Module_-_Healthy_Food_Environment_Policy_Index_Food-EPI_/5673439 (Accessed March 18, 2021).
31. Harrington, JM, Leydon, CL, Twohig, CH, and Vandevijvere, S. Policies for Tackling Obesity and Creating Healthier Food Environments in Ireland: Food-EPI 2020. Current Policies and Priority Actions (2020). Available at: https://www.jpi-pen.eu/images/reports/IE_Food-EPI%20Report_19Nov20.pdf (Accessed March 18, 2021).
32. Torheim, LE, Løvhaug, AL, Huseby, CS, and Terragni, L. Norwegian Food-EPI Report. Sunnere Matomgivelser I Norge. Vurdering Av Gjeldende Politikk Og Anbefalinger for Videre Innsats (2020). Available at: https://www.jpi-pen.eu/images/reports/FoodEPI-Report-Norway-2020.pdf (Accessed March 18, 2021).
33. Miller, D, and Harkins, C. Corporate Strategy, Corporate Capture: Food and Alcohol Industry Lobbying and Public Health. Crit Soc Pol (2010) 30(4):564–89. doi:10.1177/0261018310376805
34. Tangcharoensathien, V, Chandrasiri, O, Kunpeuk, W, Markchang, K, and Pangkariya, N. Addressing NCDs: Challenges from Industry Market Promotion and Interferences. Int J Health Pol Manag (2019) 8(5):256–60. doi:10.15171/ijhpm.2019.02
35. Mialon, M, Swinburn, B, and Sacks, G. A Proposed Approach to Systematically Identify and Monitor the Corporate Political Activity of the Food Industry with Respect to Public Health Using Publicly Available Information. Obes Rev (2015) 16(7):519–30. doi:10.1111/obr.12289
36. Ainger, K, and Klein, K. A Spoonful of Sugar. How the Food Lobby Fights Sugar Regulation in the EU (2016). Available at: https://corporateeurope.org/sites/default/files/a_spoonful_of_sugar_final.pdf (Accessed March 18, 2021).
37. Swinburn, B. Power Dynamics in 21st-century Food Systems. Nutrients (2019) 11(10):2544. doi:10.3390/nu11102544
38. Chan, M. WHO Director-General Addresses Health Promotion Conference (2013). Available at: https://www.foodpolitics.com/wp-content/uploads/DG-WHO-speech-to-Health-Promotion-Conference.pdf (Accessed March 18, 2021).
39. Moodie, R, Stuckler, D, Monteiro, C, Sheron, N, Neal, B, Thamarangsi, T, et al. Profits and Pandemics: Prevention of Harmful Effects of Tobacco, Alcohol, and Ultra-processed Food and Drink Industries. The Lancet (2013) 381(9867):670–9. doi:10.1016/s0140-6736(12)62089-3
40. Kroneman, M, Boerma, W, van den Berg, M, Groenewegen, P, de Jong, J, and van Ginneken, ENIVEL. Netherlands: Health System Review. Health Syst Transit (2016) 18(2):1–240. Available at: https://www.euro.who.int/__data/assets/pdf_file/0016/314404/HIT_Netherlands.pdf?ua=1 (Accessed March 18, 2021).
41. Peters, S, and Valkernburg, J. Former Minister Schippers of Health, Welfare and Sports (Netherlands) Interviewed about Product Reformulation: "The Healthy Choice Should Be the Easy Choice. Voeding Mag (2017) 1:1–4. Available at: https://www.researchgate.net/publication/321017078_Former_minister_Schippers_of_Health_Welfare_and_Sports_Netherlands_interviewed_about_product_reformulation_The_healthy_choice_should_be_the_easy_choice (Accessed March 18, 2021).
42.Rijksoverheid. Rijksinstituut voor Volksgezondheid en Milieu. Akkoord Verbetering Productsamenstelling. Agreements and Results (2021). Available at: https://www.akkoordverbeteringproductsamenstelling.nl/en/agreements-and-results (Accessed March 18, 2021).
43. Seidell, JC, and Halberstadt, J. National and Local Strategies in the Netherlands for Obesity Prevention and Management in Children and Adolescents. Obes Facts (2020) 13:418–29. doi:10.1159/000509588
44.Rijksoverheid Rijksinstituut voor Volksgezondheid en Milieu. Geschat effect van lagere suikergehalten in voedingsmiddelen op de dagelijkse suikerinname in Nederland (2018). Available at: https://www.rivm.nl/geschat-effect-van-lagere-suikergehalten-in-voedingsmiddelen-op-dagelijkse-suikerinname-in (Accessed March 18, 2021).
45.Rijksoverheid Rijksinstituut voor Volksgezondheid en Milieu. Geschat effect van lagere zoutgehalten in voedingsmiddelen op de dagelijkse zoutinname in Nederland (2018). Available at: https://www.rivm.nl/geschat-effect-van-lagere-zoutgehalten-in-voedingsmiddelen-op-dagelijkse-zoutinname-in-nederland (Accessed March 18, 2021).
46. Wilson, EC, Brants, HAM, Beukers, MH, and Milder, IEJ. Geschat effect van lagere zout- en suikergehalten in voedingsmiddelen op de dagelijkse zout- en suikerinname in Nederland. Akkoord verbetering productsamenstelling 2014-2020. RIVM briefrapport 2019-0231 (2019). Available at: https://www.rivm.nl/bibliotheek/rapporten/2019-0231.pdf (Accessed March 18, 2021).
47.Quickscan mogelijke impact Nationaal Preventieakkoord. Quickscan Mogelijke Impact Nationaal Preventieakkoord (2018). Available at: https://www.rivm.nl/documenten/quickscan-mogelijke-impact-nationaal-preventieakkoord (Accessed March 18, 2021).
48. Sacks, G, Swinburn, B, Kraak, V, Downs, S, Walker, C, Barquera, S, et al. A Proposed Approach to Monitor Private-Sector Policies and Practices Related to Food Environments, Obesity and Non-communicable Disease Prevention. Obes Rev (2013) 14(S1):38–48. doi:10.1111/obr.12074
49.Kamerbrief. Kamerbrief over Juridische Mogelijkheden Voor Gezonde Voedselomgeving (4 June 2021). Kenmerk 2364218-1009424-VGP (2021). Available at: https://www.rijksoverheid.nl/documenten/kamerstukken/2021/06/04/kamerbrief-over-gezonde-voedselomgeving (Accessed March 18, 2021).
50.Kabinetsformatie. Coalitieakkoord 2021 – 2025, Omzien naar elkaar, vooruitkijken naar de toekomst (15 December 2021) (2021). Available at: https://www.tweedekamer.nl/kamerstukken/detail?id=2021D50025&did=2021D50025 (Accessed December 18, 2021).
51.Stichting Reclame Code. Reclamecode Voor Voedingsmiddelen (RVV) (Updated 2019) (2021). Available at: https://www.reclamecode.nl/nrc/rvv2019/ (Accessed March 18, 2021).
52. Hawkes, C. Marketing Food to Children: Changes in the Regulatory Environment 2004-2006. Geneva, Switzerland: World Health Organization (2007). Available at: https://www.who.int/dietphysicalactivity/regulatory_environment_CHawkes07.pdf (Accessed March 18, 2021).
53.National Institute for Public Health and the Environment. ‘What’s on Our Plate? Safe, Healthy and Sustainable Diets in the Netherlands’ (2016). Available at: https://www.rivm.nl/bibliotheek/rapporten/2016-0197.pdf (Accessed March 18, 2021).
54. World Cancer Research Fund International, . NOURISHING Policy Database (2021). https://policydatabase.wcrf.org/level_one?page=nourishing-level-one (Accessed March 18, 2021).
55.Department for Digital, Culture, Media and Sport. Introducing a Total Online Advertising Restriction for Products High in Fat, Sugar and Salt (HFSS) (Updated 2020) (2020). Available at: https://www.gov.uk/government/consultations/total-restriction-of-online-advertising-for-products-high-in-fat-sugar-and-salt-hfss/introducing-a-total-online-advertising-restriction-for-products-high-in-fat-sugar-and-salt-hfss (Accessed March 18, 2021).
56. World Cancer Research Fund International, . NOURISHING Policy Database. Restrict Food Advertising and Other Forms of Commercial Promotion (2021). Availabe at: https://policydatabase.wcrf.org/level_one?page=nourishing-level-one#step2=3 (Accessed March 18, 2021).
57. World Cancer Research Fund International, . NOURISHING Policy Database. Use Economic Tools. Health-Related Food Taxes (2021). Available at: https://policydatabase.wcrf.org/level_one?page=nourishing-level-one#step2=2#step3=315 (Accessed March 18, 2021).
58.European Public Health Alliance (EPHA). Minimum VAT on Fruits and vegetables(Updated 2019) (2021). Available at: https://epha.org/living-environments-mapping-food-environments-vat/ (Accessed March 18, 2021).
59. Backholer, K, Beauchamp, A, Ball, K, Turrell, G, Martin, J, Woods, J, et al. A Framework for Evaluating the Impact of Obesity Prevention Strategies on Socioeconomic Inequalities in Weight. Am J Public Health (2014) 104(10):e43–e50. doi:10.2105/AJPH.2014.302066
60. Newman, L, Baum, F, Javanparast, S, O'Rourke, K, and Carlon, L. Addressing Social Determinants of Health Inequities through Settings: A Rapid Review. Health Promot Int (2015) 30(Suppl. 2):ii126–43. doi:10.1093/heapro/dav054
61. Raine, KD. Addressing Poor Nutrition to Promote Heart Health: Moving Upstream. Can J Cardiol (2010) 26(Suppl. C):21C–24C. doi:10.1016/s0828-282x(10)71078-3
62. Kumanyika, SK, Obarzanek, E, Stettler, N, Bell, R, Field, AE, Fortmann, SP, et al. Population-Based Prevention of Obesity. Circulation (2008) 118(4):428–64. doi:10.1161/circulationaha.108.189702
63. Løvhaug, AL, Granheim, SI, Kamphuis, CBM, Sawyer, A, Stronks, K, Poelman, MP, et al. The Potential of Food Environment Policies to Reduce Socioeconomic Inequalities in Diets and to Improve Healthy Diets Among Lower Socioeconomic Groups: an Umbrella Review. Submitted Rev BMC Public Health (2022) 1:1.
64. Olstad, DL, Teychenne, M, Minaker, LM, Taber, DR, Raine, KD, Nykiforuk, CIJ, et al. Can Policy Ameliorate Socioeconomic Inequities in Obesity and Obesity-Related Behaviours? A Systematic Review of the Impact of Universal Policies on Adults and Children. Obes ReviewsDec (2016) 17(12):1198–217. doi:10.1111/obr.12457
65. Djojosoeparto, SK, Kamphuis, CBM, Vandevijvere, S, Harrington, JM, Poelman, MP, and on behalf of the Jpi-Hdhl Policy Evaluation Network, . The Healthy Food Environment Policy Index (Food-EPI): European Union. An Assessment of EU-Level Policies Influencing Food Environments and Priority Actions to Create Healthy Food Environments in the EU. UtrechtThe Netherlands: Utrecht University (2021). Available at: https://www.jpi-pen.eu/images/reports/Food-EPI_EU_FINAL_20210305.pdf (Accessed March 18, 2021).
66.European Commission. New Rules on VAT Rates Offer Member States More Flexibility while Supporting the EU's green, Digital and Public Health Priorities. Brussels: Press release (2021). Available at: https://ec.europa.eu/commission/presscorner/detail/en/ip_21_6608 (Accessed December 18, 2021).
67. Phulkerd, S, Vandevijvere, S, Lawrence, M, Tangcharoensathien, V, and Sacks, G. Level of Implementation of Best Practice Policies for Creating Healthy Food Environments: Assessment by State and Non-state Actors in Thailand. Public Health Nutr (2016) 20(3):381–90. doi:10.1017/s1368980016002391
68. Phulkerd, S, Sacks, G, Vandevijvere, S, Worsley, A, and Lawrence, M. Barriers and Potential Facilitators to the Implementation of Government Policies on Front-Of-Pack Food Labeling and Restriction of Unhealthy Food Advertising in Thailand. Food policy (2017) 71:101–10. doi:10.1016/j.foodpol.2017.07.014
Keywords: public health, government, obesity, overweight, food environment, policies, infrastructure support
Citation: Djojosoeparto SK, Kamphuis CBM, Vandevijvere S and Poelman MP (2022) How can National Government Policies Improve Food Environments in the Netherlands?. Int J Public Health 67:1604115. doi: 10.3389/ijph.2022.1604115
Received: 26 March 2021; Accepted: 21 January 2022;
Published: 07 March 2022.
Edited by:
Serge Hercberg, Université Sorbonne Paris Nord, FranceReviewed by:
Miguel Ángel Royo-Bordonada, Carlos III Health Institute, SpainCopyright © 2022 Djojosoeparto, Kamphuis, Vandevijvere and Poelman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sanne K. Djojosoeparto, cy5rLmRqb2pvc29lcGFydG9AdXUubmw=
This Original Article is part of the IJPH Special Issue “Food as a Public Health Issue”
 Sanne K. Djojosoeparto
Sanne K. Djojosoeparto Carlijn B. M. Kamphuis
Carlijn B. M. Kamphuis Stefanie Vandevijvere
Stefanie Vandevijvere Maartje P. Poelman
Maartje P. Poelman