- 1Health Service and Population Research, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, United Kingdom
- 2Geriatric Section, Internal Medicine Department, Universidad Nacional Pedro Henriquez Ureña, Santo Domingo, Dominican Republic
- 3National Institute of Neurology and Neurosurgery of Mexico, National Autonomous University of Mexico, Mexico City, Mexico
- 4Instituto de la Memoria Depresion y Enfermedades de Riesgo, Lima, Peru
- 5Social Psychiatry and Behavioral Medicine, Institute of Mental Health, Peking University, Beijing, China
- 6Geriatrics Program, Internal Medicine Department, School of Medicine, Medical Sciences Campus, University of Puerto Rico, San Juan, Puerto Rico
- 7Facultad de Medicina Finlay-Albarran, Medical University of Havana, Havana, Cuba
- 8Medicine Department, Caracas University Hospital, Faculty of Medicine, Universidad Central de Venezuela, Caracas, Venezuela
- 9Department of Community Health, Voluntary Health Services, Chennai, India
- 10Global Health and Social Medicine, King’s Global Health Institute, Social Science and Public Policy, King’s College London, London, United Kingdom
Objectives: This study was designed to explore prevalence and correlates of self-reported loneliness and to investigate whether loneliness predicts mortality among older adults (aged 65 or above) in Latin America, China and India.
Methods: The study investigated population-based cross-sectional (2003–2007) and longitudinal surveys (follow-up 2007–2010) from the 10/66 Dementia Research Group project. Poisson regression and Cox regression analyses were conducted to analyse correlates of loneliness and its association with mortality.
Results: The standardised prevalence of loneliness varied between 25.3 and 32.4% in Latin America and was 18.3% in India. China showed a low prevalence of loneliness (3.8%). In pooled meta-analyses, there was robust evidence to support an association between loneliness and mortality across Latin American countries (HR = 1.13, 95% CI 1.01–1.26, I2 = 10.1%) and China (HR = 1.58, 95% CI 1.03–2.41), but there were no associations in India.
Conclusion: Our findings suggest potential cultural variances may exist in the concept of loneliness in older age. The effect of loneliness upon mortality is consistent across different cultural settings excluding India. Loneliness should therefore be considered as a potential dimension of public health among older populations.
Introduction
Loneliness has been described as the “unpleasant phenomenon stemming from the discrepancy between desired and achieved levels of social relations” (1). Evidence suggests loneliness may be a common experience among older people, with estimates ranging from 19.6 to 34.0% among people aged over 65 in Europe (2), and 25–29%, among participants aged 70+ years old in the United States (3). The frequency of loneliness in older age is consistent with the social effects of ageing: the accumulation of life events and processes that have the potential to destabilise social relations. For example, widowhood and onset of disability are more likely in older age (1) and personal and friendship networks decrease throughout adulthood (4). Loneliness is a subjective evaluation of an individual’s context which is made up of perceived deficits in social contacts and unmet social needs, which can be affected by both quantity and quality of personal relationships (5). Social isolation is a related concept which reflects an objective condition of lacking integration into social networks and social contacts, which is commonly associated with loneliness. However, the concepts are not interchangeable: it is not necessary to be socially isolated in order to experience loneliness (6).
Research carried out in high income country (HIC) settings has consistently identified sociodemographic correlates of loneliness: female gender (7, 8), older age (8), low educational level (9), poor income (10), being widowed (11, 12), living alone and low quality of social relationships (8, 11); as well as a number of adverse health outcomes, such as low well-being (12), mobility difficulties (12, 13), chronic diseases (14), cardiovascular ill-health (15, 16), depression and dementia (5). Direction of causality has been difficult to ascertain. This is due to the cross-sectional design of most studies as well as the possibility of reverse causality, which, due to the likely complexity of the relationships between factors such as depression, is often retained, even in the context of longitudinal designs (16). Evidence about the effect of loneliness on mortality in older adults is also mixed (16). Findings from studies carried out in Western Europe, United States and China suggest that loneliness has an independent effect upon mortality, with hazard ratios (HRs) ranging from 1.45 (95% CI 1.11–1.88) in the United States (17) to 1.17 (95% CI 1.02–1.33) in Finland (18).
Many of the factors thought to influence loneliness among older people (age, gender, widowhood, quality of social relationships) have been found to be relevant across different cultural settings (19). Qualitative findings from low- and middle-income countries (LMICs) have revealed similar narratives among older people: with change in family/social relationships like loss of spouses, being separated, reduced decision-making power and autonomy within the family, living alone and reduced social connections identified as the circumstances which shape experiences of loneliness (20–23). However, cultural differences in conceptions of the roles of older people, familial relationships and broader societal differences may potentially result in variation in experience and reporting of loneliness (24). Given the expected roles of culture and context in shaping experience of older age, findings about the effects of loneliness are not necessarily transferable across settings. We did not identify any studies which compared differences in loneliness prevalence and correlates across different cultural settings. Given the possible importance of loneliness as a potentially modifiable predictor of adverse outcomes including mortality (16, 18, 25), there is a need for research which examines loneliness in different cultural settings.
Using data from the 10/66 Dementia Research Group (10/66 DRG) study collected in Latin America, China and India, our analysis addresses three objectives related to gaining a better understanding of loneliness among older people in LMICs: 1) To estimate the prevalence of loneliness; 2) To examine whether correlates of loneliness identified from the literature were associated with the measure of loneliness used in the 10/66 DRG studies across different cultural settings; 3) To test the hypothesis that, after adjustment for sociodemographic and health-related correlates, loneliness was independently associated with mortality.
Methods
Context and Data Resources
The study is a secondary data analysis using population-based cross-sectional and longitudinal surveys from the 10/66 DRG project. The surveys were conducted among older adults (aged 65 or above) living in 12 geographically defined catchment areas in eight countries, including Cuba (Havana/Matanzas-urban), Dominican Republic (Santo Domingo-urban), Puerto Rico (Bayamon-urban), Venezuela (Caracas-urban), Peru (Lima-urban & Canete Province-rural), Mexico (Mexico City-urban and Morelos state-rural), China (Xicheng-urban and Daxing-rural) and India (Chennai-urban and Vellore-rural). Catchment areas were defined geographic areas selected for accessibility (26, 27). All assessments used in field work have been translated into relevant local languages (Ibero-American Spanish, Tamil and Mandarin). Baseline data were collected between 2003 and 2007, with high response rates for the baseline surveys across sites (72–98%). All participants were interviewed and assessed comprehensively, with interviews lasting around 2–3 h. For those lacking capacity of consent or with communication difficulties caused by dementia, mental or physical illnesses, informants were interviewed about the older person. The follow-up surveys were conducted between 2007 and 2010, which attempted to trace and re-interview all baseline study participants with at least three times visits were considered as untraced. Participants who moved outside the original catchment areas were re-interviewed in follow-up survey as well. Follow-up surveys were carried out in all baseline study sites except for the rural study site in India. The original study ethical approval was obtained from local ethical committees and the King’s College London Research Ethics Committee. A detailed protocol has been published elsewhere (28).
Measures
Exposure
Information on self-reported experience of loneliness was assessed by a single item on the Geriatric Mental State (GMS)-Automated Geriatric Examination for Computer Assisted Taxonomy (AGECAT) package (29): “Do you feel lonely?,” with three response options (“no”/“yes but mild to moderate intensity, infrequent or fleeting”/“yes and severe, frequent or persistent”). The assessment of loneliness was coded as “feeling lonely” if the item was rated positive and recoded into a binary variable (yes/no). Single-item measures of loneliness have been commonly used in population-based studies across different cultural settings (30, 31).
Outcome
Vital status of older participants was ascertained during the initial “door-knocking” process, carried out with all households who participated in baseline surveys, to assess changes to households during the follow-up period. The starting of the risk time was dates of the baseline survey. The date of death, the date of follow-up for re-interviewed participants who moved away from the original catchment areas, or the median date of follow-up for participants who refused the interview was recorded and censored as survival time (28, 32).
Covariates
Socio-demographic information on age, gender, marital status, education, pension and wealth were assessed by a standard socioeconomic demographic questionnaire. Age was measured as a continuous variable, and recoded into four bands (65–69, 70–74, 75–79, 80+) for analyses; marital status categorised into four groups (never married, married/co-habiting, widowed, divorced/separated); level of education was classified as five groups (none, incomplete primary, completed primary, completed secondary (metric), and completed tertiary (college)/further education). Pension was a dichotomous variable, assessed by whether older people received any government or occupational pension; household assets index was recorded by summing up the number of household assets owned (i.e., car, television, refrigerator, telephone, mains electricity, mains water, plumbed toilet) and recoded into four quarters, which used to as an indicator for older people’s wealth. Social network types were operationally assessed and generated into Wenger’s network typology by using the Practitioner Assessment of Network Type (PANT), as a categorical variable including locally integrated, locally self-contained, wider community focused, family dependent and private network types. The locally integrated support network type represents the widest access to social support, whilst the private network type refers to the narrowest network type, which can be described as an absence of local or nearby family and friends and with low levels of community contact or involvement. The details of social network measurement, algorithm and explanation have been described elsewhere (33). Whether participants lived alone was a single item question (yes/no).
Physical impairments were assessed through a self-reported list of 11 common physical impairments (i.e., arthritis or rheumatism; eyesight problems; hearing difficulties or deafness; persistent cough; breathlessness, difficulty breathing or asthma; high blood pressure; heart trouble or angina; stomach or intestine problems; faints or blackouts; paralysis, weakness or loss of one leg or arm; skin disorders) and recoded and categorised as “no impairments,” “one to two impairments,” and “three or more impairments” (32). Care dependence was assessed by asking open-ended questions to the key informant about participant’s needs for care and then coded by interviewers and categorised as “required no care” or “care some” or “need much care”, which was used here to define “dependence” at both baseline and follow-up surveys (26). Depression was measured by structured clinical interview (the GMS), and derived from its computerised algorithm AGECAT, which provided International Classification of Diseases-10 (ICD-10) depressive episode diagnoses (mild/moderate/severe) (29, 34). Dementia was ascertained by either the cross-culturally validated 10/66 dementia diagnosis algorithm or DSM-IV (Diagnostic and Statistical Manual of Mental Disorders) dementia diagnostic criterion (35–37).
Statistical Analysis
All analyses were conducted using STATA version 15 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.). Initial analyses were presented on the prevalence and correlates of self-reported loneliness in the baseline dataset. 346 participants who did not respond to the loneliness question were excluded from our analyses (Cuba n = 47; Dominican Republic n = 11; Peru n = 49; Venezuela n = 21; Mexico n = 11; Puerto Rico n = 95; China n = 61; India n = 51). No follow-up survey was conducted in the rural site of India hence participants from this site were excluded in the mortality analyses. A weighting variable was provided by the 10/66 DRG baseline dataset for each country for direct standardisation, with the whole sample as the standard population. The crude and direct standardised prevalence of loneliness adjusted for age, gender and education with robust 95% confidence intervals (CI) was estimated by accounting for household clustering across the whole sample as well as within each country. We used Poisson regression models to examine all hypothesised and theory-driven correlates of loneliness in each country, by adjusting for age, gender, education, household assets, pension, marital status, social network, living alone, physical impairments, care dependence, depression and dementia. The adjusted prevalence ratios (PRs) (with robust 95% CI) for loneliness were reported separately for each country, and then pooled with fixed effect meta-analysis across all study sites combined and Latin American countries.
Kaplan-Meier curves were generated to compare crude mortality between participants with and without loneliness. The differences between the survival curves were tested using Log-rank tests. Univariate and Multivariable Cox proportional hazards regression models were conducted to examine the association between loneliness and mortality, while the Schoenfeld residuals test was used to test the proportional hazard assumptions. Multivariable Cox models were built based on a combination of literature review, results from bivariate analysis and consideration of distribution of characteristics. Variables were gradually added in blocks. Blocks were determined from background literature, based on knowledge of factors associated with loneliness (sociodemographic, social isolation, physical health, mental health). Variables were selected for inclusion in blocks if considered as potential confounders on the basis of being correlated with loneliness in bivariate analyses. Three sets of models were built: for Latin American countries, India and for China. Across six Latin American countries and India, models were ultimately adjusted for (Model I) baseline socio-demographic factors (age, gender, education and household assets), then (Model II) adding social network, followed by (Model III) adding dependence; finally (Final Model) depression and dementia were included. Considering building the model for China, previous 10/66 DRG studies based on the same samples showed that there was no association between social network and mortality in the adjusted model for China. As only family dependent social network type showed an association in the unadjusted model in for the Chinese 10/66 baseline dataset (33), and living alone played a role in reflecting family connections and marital status, we decided to include living alone instead of social network in Multivariable Cox model building for China in this study. Finally, we introduced time-varying interactions for age and education for fitting our Cox models for China. The likelihood ratio test was used to test the fit of each model. The adjusted HRs for loneliness were reported and fitted in each site separately and then combined with fixed effect meta-analysis to generate pooled HRs across Latin American countries. Higgins I2 was measured to estimate the level of heterogeneity across the estimates in different settings. Lower than 40% heterogeneity was considered as negligible, and 40–60% was regarded as moderate heterogeneity (38).
Results
Baseline Characteristics of Study Samples and Vital Status at Follow Up
A total of 16,685 older adults (65 years and above) were included in the baseline sample across eight LMICs. Sample numbers were around 2000 (ranging from 2,897 to 1,884) in each study country except Cuba which had a slightly larger sample (n = 2,897). The mean age of participants was 74.1 (6.9) years and evenly distributed across the five bands, except that in three sites (Venezuela, China and India), there were proportionately fewer in the oldest age category. Overall, 62.4% of samples were female. Across countries the female proportion exceeded the male but was distributed evenly (Supplementary File S1). 13,673 (86.9%) of 15,733 participants interviewed at baseline participated in follow-up (re-interviewed or vital status ascertained). There were some differences in the loss to follow-up rates by baseline loneliness status in study countries (14.6% for loneliness vs. 12.6% without loneliness), especially for Cuba, Venezuela and China (p < 0.05). 2,439 participants were recorded dead, which accounted for 17.8% of those successfully traced. Overall, median follow-up years was 4.0 years (3.0–4.9), equivalent to a total of 53,139.4 person years of follow-up. The proportion of baseline participants where vital status was ascertained was evenly distributed across countries. Mortality was highest in Dominican Republic (27.1%), followed by China, Cuba and India, which were higher than other countries. Differences in timing of data collection in each country led to a variance on follow-up years, with median follow-up years shorter in India, Mexico and Peru (Table 1).
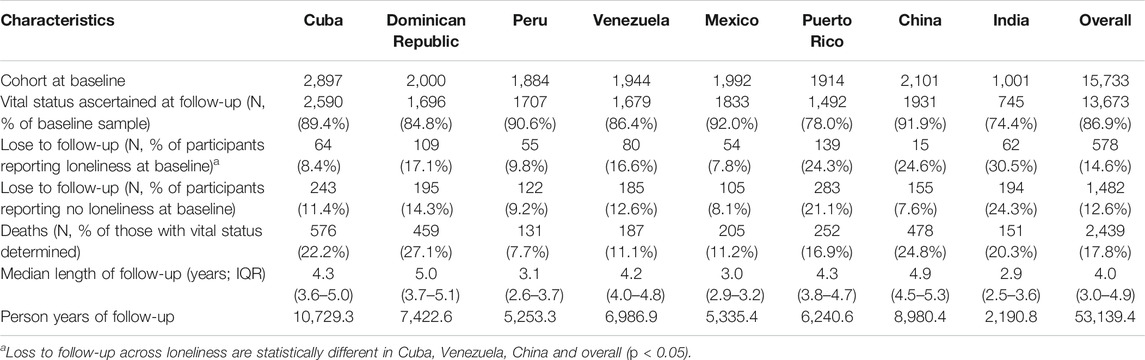
TABLE 1. Characteristics of vital status at follow up for those whose vital status was known (The 10/66 Dementia Research Group study 2003–2010).
Prevalence of Loneliness and Its Correlates
The standardised prevalence of loneliness varied between 25.3 and 32.4% by Latin American countries. The highest standardised prevalence of loneliness was 32.4% (95%CI 29.9–34.8%) in Mexico, followed by Puerto Rico 32.2% (95% CI 29.0–35.4%). The standardised prevalence of loneliness was lower in India (18.3%, 95% CI 16.0–20.6%) compared to Latin American countries, whilst China showed an extremely low prevalence (3.8%, 95% CI 2.6–4.9%) (Table 2). According to the results of Multivariable Poisson regression, pooled adjusted PR for loneliness showed that, across all countries, loneliness was significantly associated with female gender, lower education level, lower household assets index, being widowed (pooled PR = 1.31, 95% CI 1.17–1.46, I2 = 36.5%) or divorced/separated (pooled PR = 1.27, 95% CI 1.13–1.43, I2 = 0%), with a narrower social network type, living alone (pooled PR = 1.42, 95% CI 1.32–1.52, I2 = 51.5%), with more physical impairments, with care dependence, depression and dementia. Compared to people with locally integrated social network, participants with private social network had a significant association with loneliness (pooled PR = 1.14, 95% CI 1.03–1.27, I2 = 43.4% all countries combined; pooled PR = 1.20, 95% CI 1.07–1.35, I2 = 38.2%, Latin American countries combined). Pooled PR for more physical impairments was 1.32 (95% CI 1.27–1.37, I2 = 32.8%, all countries combined). Older people with care dependence were correlated with feeling lonely (pooled PR = 1.14, 95% CI 1.02–1.27, I2 = 0% all countries combined; pooled PR = 1.13, 95% CI 1.0–1.26, I2 = 16.0%, Latin American countries combined). Depression showed a significant pooled effect on loneliness (pooled PR = 1.95, 95% CI 1.83–2.07, I2 = 73.2% across all countries; pooled PR = 1.92, 95% CI 1.79–2.06, I2 = 0%, Latin American countries combined) (Table 3). The adjusted PRs for loneliness were reported separately for study site in Supplementary File S2.
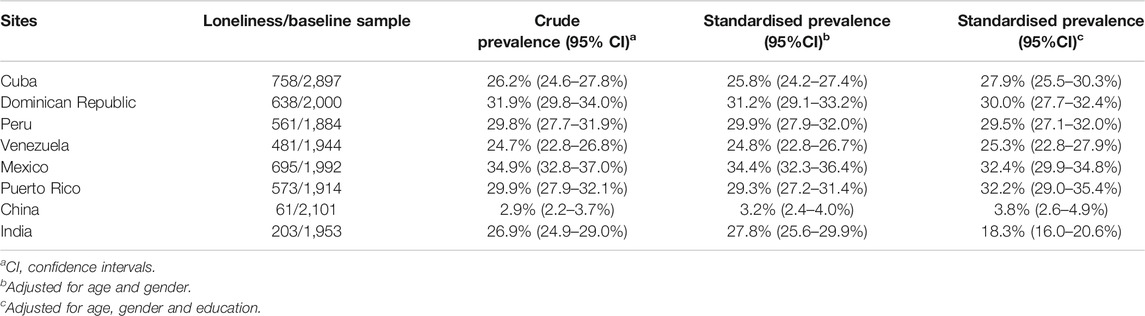
TABLE 2. Crude and standardised prevalence of self-reported loneliness in Latin America, China, and India (The 10/66 Dementia Research Group study 2003–2007).
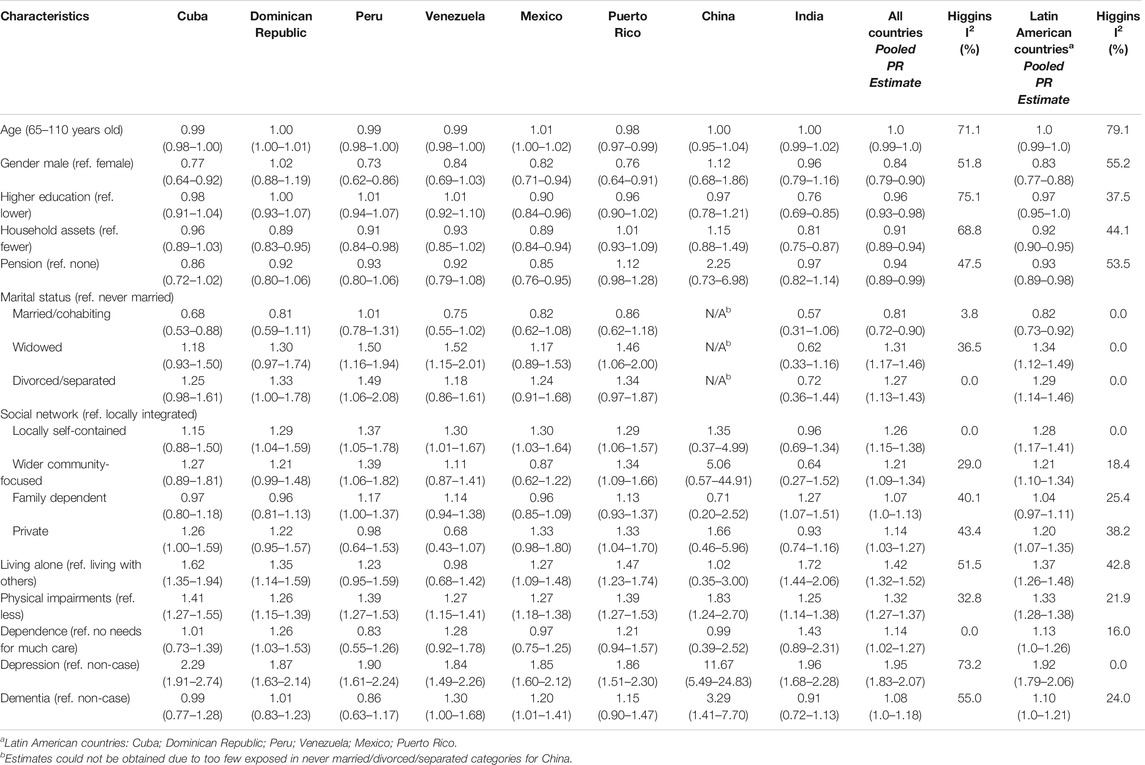
TABLE 3. Correlates of loneliness with adjusted prevalence ratios (robust 95% confidence interval) in Latin America, China, and India (The 10/66 Dementia Research Group study 2003–2007).
Loneliness and Mortality
Crude Kaplan-Meier curves showed that participants with loneliness at baseline had lower 5-year survival rates (Figure 1), and with no difference between both gender and age strata (Supplementary File S3). Kaplan-Meier curves were plotted for the original three responses measure of loneliness, which showed a potential dose-response effect of increasing loneliness status (Supplementary File S4). Log-rank test gave p < 0.05 in all curves. Results of multivariable Cox models for Latin American countries, China and India showed that when restricted to Latin American countries pooled, the crude HR for loneliness was 1.25 (95% CI 1.14–1.38), with a moderate level of heterogeneity (I2 = 43.9%). In the final pooled analysis, after adjustment for all potential confounders, there was evidence for an association between loneliness and mortality (pooled adjusted HR = 1.13, 95% CI 1.01–1.26, I2 = 10.1%). In India, there was no association between loneliness and mortality across all models. However, in China, the effect of loneliness on mortality risk remained strong in the final model after adjusting for all confounders (adjusted HR = 1.58, 95% CI 1.03–2.41) (Table 4). Schoenfeld residuals test, p > 0.05 for all Cox models in Table 4.
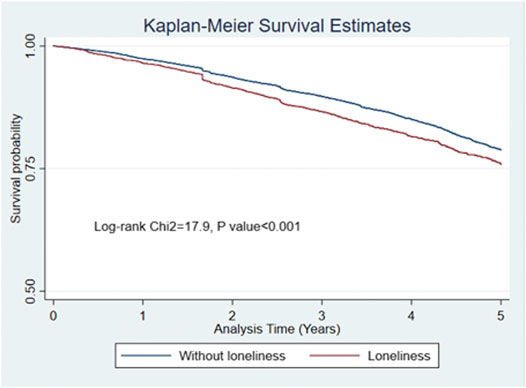
FIGURE 1. Kaplan-Meier survival curve for 5-year all-cause mortality, stratified by self-reported loneliness (The 10/66 Dementia Research Group study 2003-2010).
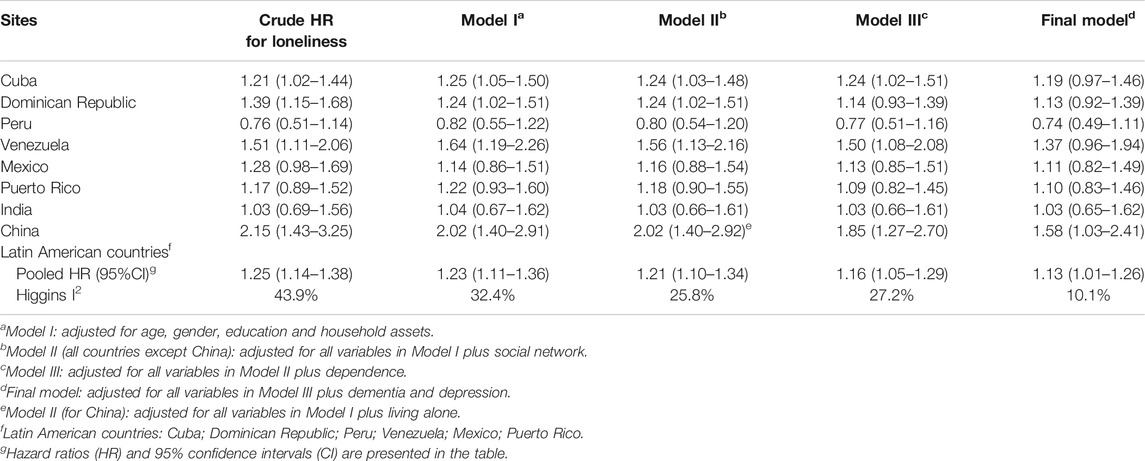
TABLE 4. Meta-analysed pooled effect sizes for the association between loneliness and mortality in Latin America, China, and India (The 10/66 Dementia Research Group study 2003–2010).
Discussion
The study found that the age, gender and education- standardised prevalence of loneliness ranged from 25.3% to 32.4% across Latin American countries, consistent with findings from the European Social Survey (2006–2007), which reported similar prevalence estimates of loneliness using a single-item measure with prevalence estimates ranging between 19.6% and 34.0% for older people aged 60 years old and above (2). In our study, we found a much lower standardised prevalence of loneliness in China of 3.8% compared to the 29.6% prevalence among older adults identified by a Chinese national ageing survey in 2000 (39). Although it is possible that the difference between our results and the nationally representative survey may reflect a real difference in levels of loneliness in the 10/66 DRG catchments, this result may be an artefact of our single item approach to measurement, a limitation which we discuss in more detail below. Our study showed that the direct standardised prevalence of loneliness was 18.3% in India, but there was scant previous evidence about the prevalence of loneliness among Indian elderly. The prevalence estimates of loneliness in this study showed a more similar pattern across Latin American countries, whereas lower prevalence was observed in China and India. Similar differences on prevalence of anxiety (40) and amnestic mild cognitive impairment (41) were observed in previous 10/66 DRG findings, where both studies reported a low prevalence in China. As applying a cross-cultural approach through using the same study design, sampling and measurements in this study, the inconsistence of prevalence estimates on the subjective feeling of loneliness across study countries is likely due to the measure of self-reported loneliness itself, as cultural variances may influence the conception of loneliness and stigma (41).
The hypothesis that loneliness increased mortality was supported by our results and was consistent across all countries except India. In Latin American countries, we found that after adjustment for all the sociodemographic and health-related confounders, pooled estimates still suggested robust evidence on an association between loneliness and mortality, consistent with the results of previous meta-analyses (42, 43). Whilst depression is undoubtedly associated with loneliness and vice versa (44), there is evidence to suggest that both depression and loneliness have independent effects on mortality despite common co-existence. In our study, adding depression and dementia to the model made very little difference to our results, thereby suggesting an independent association of loneliness to mortality. Despite a low prevalence, we found a strong association between loneliness and mortality in China, which was retained after adjustment for the same sets of characteristics. This might reveal the possibility that our measurement captured more intense cases of loneliness, but this remains untested. Both direct and indirect pathways have been posited as explanations for associations between loneliness and mortality in previous research. Indirect mechanisms include circular relationships between loneliness and behaviours (smoking, physical inactivity, poorer sleep) (44, 45) associated with poor health and their subsequent effects upon physiological outcomes; whilst direct mechanisms include emerging evidence to suggest that levels of social support may be linked to immune-mediated inflammatory processes (46).
Our findings regarding correlates were generally consistent with the literature from studies carried out in HIC settings. Older people, being female, living without a spouse, living alone, and those with lower socioeconomic status were more likely to be lonely. These factors often cluster together within individuals, are interrelated (e.g., form a “vicious cycle”) and are associated with low mood, a sense of meaninglessness or hopelessness as well as loneliness (20, 47). Locally integrated networks were most protective in terms of loneliness, whilst being dependent on others, having physical impairments, dementia and depression were all associated with loneliness. The results of qualitative work carried out in 10/66 sites and elsewhere offer further insight into the context in which loneliness in older age might emerge. Consistent with our current findings, a recent systematic review of qualitative studies from LMICs showed that loneliness was often characterised by older people as loss: of physical functioning, independence, close confidantes, social participation and sense of belonging within families and societies (20, 22, 23). Results from the 10/66 DRG INDEP study and a recent study in Ghana carried out among dependent older people suggest that changing societal expectations (greater female participation in paid employment, longer periods of education for young people) were putting a strain on social norms of intergenerational reciprocity (48, 49).
A key potential limitation of our study was that the measure of loneliness in this study was based on self-report of a single item. Although single-item measures of loneliness are commonly used, the validity of this approach has been questioned (3, 50). Compared to multi-item scales which capture variations in frequency and intensity of loneliness across different dimensions of the phenomenon, single-item measures risk under-reporting through simplification of the construct. This limitation might perhaps be considered particularly salient in cultural settings where loneliness might be associated with stigma and shame (22). In addition, a single item is unlikely to detect culturally mediated expressions of loneliness which may be conceptually linked but not recognised or labelled as “loneliness” by study participants. Nonetheless, the broad consistency of our findings with the literature regarding demographic, social and health factors associated with loneliness is reassuring, providing evidence to support concurrent validity of the measure. The reason for a single item measure detecting such a low prevalence of loneliness among our China sample remains unexplained and warrants further investigation. Given the low attrition overall, whilst we acknowledge the presence of differential loss to follow-up, we estimate the overall impact on our final results to be minimal. Our modelling strategy was guided by evidence developed from review of the literature. Constrained by secondary data analysis and available data, we cannot rule out the possibility that the association between mortality and loneliness was explained by unmeasured confounders. Although marital status, living alone and social network (to represent social relationships) were included in the analysis, it is unclear to what extent these variables capture the social reality of participants. Finally, in this cross cultural and population-based study, it is hard to eliminate missing data and loss to follow up, which might also lead to some limited selection bias as well as limiting the generalisability of the results to some extent.
The results of our study suggest that as is now the case in HICs, loneliness in LMICs among older populations should be considered a potential public health concern. We have demonstrated a significant minority of older people experience loneliness across diverse settings and that this construct has the expected associations with other demographic, social and health-related characteristics. We have shown that loneliness has a consistent effect upon mortality, independent of the effects of sociodemographic background, social network and mental health. Further research will be needed to understand the relationship between loneliness and health among older people in LMICs. Our results highlight the importance of considering social reality in the design of interventions designed to improve the health of older people. Although instrumental support and policies designed to facilitate this are undoubtedly needed, interventions targeting health outcomes will be missing opportunities to improve the lives of older people if they don’t consider the social dimensions of ageing, such as loneliness (24, 51).
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: the 10/66 Dementia Research Group (https://1066.alz.co.uk) established an anonymised data sharing archive with monitored public access.
Ethics Statement
The studies involving human participants were reviewed and approved by King’s College London Research Ethics Committee and all local ethical committees: Memory, Depression Institute and Risk Diseases (IMEDER) Ethics Committee (Peru); Finlay Albarran Medical Faculty of Havana Medical University Ethical Committee (Cuba); Hospital Universitario de Caracas Ethics Committee (Venezuela); Consejo Nacional de Bioética y Salud (CONABIOS, Dominican Republic); Instituto Nacional de Neurología y Neurocirugía Ethics Committee (Mexico); Oficina para la Protección de Participantes Humanos en Investigación (OPPHI, Puerto Rico); Peking University Institute of Mental Health Ethics Committee (China). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors contributed to the development of the work. MP led the research group. DA (Dominican Republic), AL (Mexico), MG (Peru), YH (China), IJ-V (Puerto Rico), JL (Cuba), AS (Venezuela), JW (Chennai, India), and YH were principal investigators responsible for the fieldwork in 10/66 DRG research countries. ZL (China) and IA (Mexico) were worked as coordinators of the 10/66 DRG research group. QG developed research protocol, conducted the analyses and wrote the first draft of the manuscript under the supervision of RM and AMP. All authors read and approved the final manuscript.
Funding
The Wellcome Trust Health Consequences of Population Change Program funded the population-based prevalence phase (GR066133) and the incidence phase in Peru, Mexico, Argentina, Cuba, Dominican Republic, Venezuela, and China (GR08002). The World Health Organization funded the prevalence phase in India, Dominican Republic, and China. The United States Alzheimer’s Association funded the prevalence phase in Peru and Mexico (IIRG-04-1286). Alzheimer’s Disease International has provided support for networking and infrastructure for the 10/66 Dementia Research Group. The funding bodies had no role in the study design and the collection, analysis, and interpretation of data.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2021.604449/full#supplementary-material.
References
1. Perlman, D, and Peplau, LA. Loneliness. In: H Friedman, editor. Encyclopedia of mental health. Vol. 2. San Diego, CA: Academic Press (1998). p. 571–81.
2. Yang, K, and Victor, C. Age and loneliness in 25 European nations. Ageing Soc (2011). 31(8):1368–88. doi:10.1017/s0144686x1000139x
3. Ong, AD, Uchino, BN, and Wethington, E. Loneliness and health in older adults: a mini-review and synthesis. Gerontology (2016). 62(4):443–9. doi:10.1159/000441651
4. Wrzus, C, Hänel, M, Wagner, J, and Neyer, FJ. Social network changes and life events across the life span: a meta-analysis. Psychol Bull (2013). 139(1):53–80. doi:10.1037/a0028601
5. De Jong Gierveld, J, and Havens, B. Cross-national comparisons of social isolation and loneliness: introduction and overview. Can J Aging (2004). 23(2):109–13. doi:10.1353/cja.2004.0021
6. Rook, KS. Research on social support, loneliness, and social isolation: toward an integration. Rev Pers Soc Psychol (1984). 5:239–64.
7. Dahlberg, L, Andersson, L, McKee, KJ, and Lennartsson, C. Predictors of loneliness among older women and men in Sweden: a national longitudinal study. Aging Mental Health (2015). 19(5):409–17. doi:10.1080/13607863.2014.944091
8. Cohen-Mansfield, J, Hazan, H, Lerman, Y, and Shalom, V. Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int Psychogeriatr (2016). 28(4):557–76. doi:10.1017/s1041610215001532
9. Dykstra, PA, and de Jong Gierveld, J. Differential indicators of loneliness among elderly. The importance of type of partner relationship, partner history, health, socioeconomic status and social relations. Tijdschr Gerontol Geriatr (1999). 30(5):212–25.
10. Luanaigh, CÓ, and Lawlor, BA. Loneliness and the health of older people. Int J Geriat Psychiatry (2008). 23(12):1213–21. doi:10.1002/gps.2054
11. Victor, CR, Scambler, SJ, Bowling, A, and Bond, J. The prevalence of, and risk factors for, loneliness in later life: a survey of older people in Great Britain. Ageing Soc (2005). 25(6):357–75. doi:10.1017/s0144686x04003332
12. Dahlberg, L, and McKee, KJ. Correlates of social and emotional loneliness in older people: evidence from an English community study. Aging Mental Health (2014). 18(4):504–14. doi:10.1080/13607863.2013.856863
13. Cohen-Mansfield, J, and Parpura-Gill, A. Loneliness in older persons: a theoretical model and empirical findings. Int Psychogeriatr (2007). 19(2):279–94. doi:10.1017/s1041610206004200
14. Richard, A, Rohrmann, S, Vandeleur, CL, Schmid, M, Barth, J, and Eichholzer, M. Loneliness is adversely associated with physical and mental health and lifestyle factors: results from a Swiss national survey. PLoS One (2017). 12(7):e0181442. doi:10.1371/journal.pone.0181442
15. Hawkley, LC, Thisted, RA, Masi, CM, and Cacioppo, JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging (2010). 25(1):132–41. doi:10.1037/a0017805
16. Courtin, E, and Knapp, M. Social isolation, loneliness and health in old age: a scoping review. Health Soc Care Community (2017). 25(3):799–812. doi:10.1111/hsc.12311
17. Perissinotto, CM, Stijacic Cenzer, I, and Covinsky, KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med (2012). 172(14):1078–83. doi:10.1001/archinternmed.2012.1993
18. Tilvis, RS, Laitala, V, Routasalo, PE, and Pitkälä, KH. Suffering from loneliness indicates significant mortality risk of older people. J Aging Res (2011). 2011:534781. doi:10.4061/2011/534781
19. Luo, Y, and Waite, LJ. Loneliness and mortality among older adults in China. J Gerontol B Psychol Sci Soc Sci (2014). 69(4):633–45. doi:10.1093/geronb/gbu007
20. Roos, V, and Klopper, H. Older persons’ experiences of loneliness: a South African perspective. J Psychol Africa (2010). 20(2):281–9. doi:10.1080/14330237.2010.10820377
21. Lou, VWQ, and Ng, JW. Chinese older adults’ resilience to the loneliness of living alone: a qualitative study. Aging Mental Health (2012). 16(8):1039–46. doi:10.1080/13607863.2012.692764
22. Heravi-Karimooi, M, Anoosheh, M, Foroughan, M, Sheykhi, MT, and Hajizadeh, E. Understanding loneliness in the lived experiences of Iranian elders. Scand J Caring Sci (2010). 24(2):274–80. doi:10.1111/j.1471-6712.2009.00717.x
23. Van Der Geest, S. “They don’t come to listen”: the experience of loneliness among older people in Kwahu, Ghana. J Cross Cult Gerontol (2004). 19(2):77–96. doi:10.1023/b:jccg.0000027846.67305.f0
24.World Health Organization. Global health and ageing. Geneva, Switzerland: World Health Organization (2011). Available from: https://www.who.int/ageing/publications/global_health.pdf Accessed 25 April 2019.
25. Tilvis, RS, Routasalo, P, Karppinen, H, Strandberg, TE, Kautiainen, H, and Pitkala, KH. Social isolation, social activity and loneliness as survival indicators in old age; a nationwide survey with a 7-year follow-up. Eur Geriatr Med (2012). 3(1):18–22. doi:10.1016/j.eurger.2011.08.004
26. Prina, AM, Acosta, D, Acosta, I, Guerra, M, Huang, Y, Jotheeswaran, AT, et al. Cohort profile: the 10/66 study. Int J Epidemiol (2017). 46(2):406–406i. doi:10.1093/ije/dyw056
27. Prina, AM, Mayston, R, Wu, Y-T, and Prince, M. A review of the 10/66 dementia research group. Soc Psychiatry Psychiatr Epidemiol (2019). 54(1):1–10. doi:10.1007/s00127-018-1626-7
28. Prince, M, Ferri, CP, Acosta, D, Albanese, E, Arizaga, R, Dewey, M, et al. The protocols for the 10/66 dementia research group population-based research programme. BMC Public Health (2007). 7:165. doi:10.1186/1471-2458-7-165
29. Copeland, JRM, Dewey, ME, and Griffiths-Jones, HM. A computerized psychiatric diagnostic system and case nomenclature for elderly subjects: GMS and AGECAT. Psychol Med (1986). 16(1):89–99. doi:10.1017/s0033291700057779
30. Tan, JH, Abdin, E, Shahwan, S, Zhang, Y, Sambasivam, R, Vaingankar, JA, et al. Happiness and cognitive impairment among older adults: investigating the mediational roles of disability, depression, social contact frequency, and loneliness. Int J Environ Res Public Health (2019). 16(24):4954. doi:10.3390/ijerph16244954
31. Holwerda, TJ, Deeg, DJH, Beekman, ATF, van Tilburg, TG, Stek, ML, Jonker, C, et al. Feelings of loneliness, but not social isolation, predict dementia onset: results from the Amsterdam Study of the Elderly (AMSTEL). J Neurol Neurosurg Psychiatry (2014). 85(2):135–42. doi:10.1136/jnnp-2012-302755
32. Jotheeswaran, J, Bryce, R, Prina, M, Acosta, D, Ferri, CP, Guerra, M, et al. Frailty and the prediction of dependence and mortality in low- and middle-income countries: a 10/66 population-based cohort study. BMC Med (2015). 13:138. doi:10.1186/s12916-015-0378-4
33. Santini, ZI, Koyanagi, A, Tyrovolas, S, Haro, JM, Fiori, KL, Uwakwa, R, et al. Social network typologies and mortality risk among older people in China, India, and Latin America: a 10/66 Dementia Research Group population-based cohort study. Soc Sci Med (2015). 147:134–43. doi:10.1016/j.socscimed.2015.10.061
34. Sousa, RM, Ferri, CP, Acosta, D, Albanese, E, Guerra, M, Huang, Y, et al. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey. Lancet (2009). 374(9704):1821–30. doi:10.1016/s0140-6736(09)61829-8
35. Prince, M, Acosta, D, Chiu, H, Scazufca, M, and Varghese, M. Dementia diagnosis in developing countries: a cross-cultural validation study. Lancet (2003). 361(9361):909–17. doi:10.1016/s0140-6736(03)12772-9
36. Rodriguez, JJL, Ferri, CP, Acosta, D, Guerra, M, Huang, Y, Jacob, K, et al. Prevalence of dementia in Latin America, India, and China: a population-based cross-sectional survey. Lancet (2008). 372(9637):464–74. doi:10.1016/s0140-6736(08)61002-8
37. Prince, M, Acosta, D, Chiu, H, Copeland, J, Dewey, M, Scazufca, M, et al. Effects of education and culture on the validity of the Geriatric Mental State and its AGECAT algorithm. Br J Psychiatry (2004). 185:429–36. doi:10.1192/bjp.185.5.429
38. Higgins, JPT, and Thompson, SG. Quantifying heterogeneity in a meta-analysis. Stat Med (2002). 21(11):1539–58. doi:10.1002/sim.1186
39. Yang, K, and Victor, CR. The prevalence of and risk factors for loneliness among older people in China. Ageing Soc (2008). 28(3):305–27. doi:10.1017/s0144686x07006848
40. Prina, AM, Ferri, CP, Guerra, M, Brayne, C, and Prince, M. Prevalence of anxiety and its correlates among older adults in Latin America, India and China: cross-cultural study. Br J Psychiatry (2011). 199(6):485–91. doi:10.1192/bjp.bp.110.083915
41. Sosa, AL, Albanese, E, Stephan, BCM, Dewey, M, Acosta, D, Ferri, CP, et al. Prevalence, distribution, and impact of mild cognitive impairment in Latin America, China, and India: a 10/66 population-based study. PLoS Med (2012). 9(2):e1001170. doi:10.1371/journal.pmed.1001170
42. Rico-Uribe, LA, Caballero, FF, Martin-Maria, N, Cabello, M, Ayuso-Mateos, JL, and Miret, M. Association of loneliness with all-cause mortality: a meta-analysis. PLoS One (2018). 13(1):e0190033. doi:10.1371/journal.pone.0190033
43. Holt-Lunstad, J, Smith, TB, Baker, M, Harris, T, and Stephenson, D. Loneliness and social isolation as risk factors for mortality. Perspect Psychol Sci (2015). 10(2):227–37. doi:10.1177/1745691614568352
44. Hawkley, LC, and Cacioppo, JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med (2010). 40(2):218–27. doi:10.1007/s12160-010-9210-8
45. Kobayashi, LC, and Steptoe, A. Social isolation, loneliness, and health behaviors at older ages: longitudinal cohort study. Ann Behav Med (2018). 52(7):582–93. doi:10.1093/abm/kax033
46. Uchino, BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med (2006). 29(4):377–87. doi:10.1007/s10865-006-9056-5
47. Zhang, W, Liu, L, Tang, F, and Dong, X. Social engagement and sense of loneliness and hopelessness: findings from the PINE study. Gerontol Geriatr Med (2018). 4:2333721418778189. doi:10.1177/2333721418778189
48. Agyeman, N, Guerchet, M, Nyame, S, Tawiah, C, Owusu-Agyei, S, Prince, MJ, et al. “When someone becomes old then every part of the body too becomes old”: experiences of living with dementia in Kintampo, rural Ghana. Transcult Psychiatry (2019). 56:895–917. doi:10.1177/1363461519847054
49. Mayston, R, Lloyd-Sherlock, P, Gallardo, S, Wang, H, Huang, Y, Montes de Oca, V, et al. A journey without maps—understanding the costs of caring for dependent older people in Nigeria, China, Mexico and Peru. PLoS One (2017). 12(8):e0182360. doi:10.1371/journal.pone.0182360
50. Shiovitz-Ezra, S, and Ayalon, L. Use of direct versus indirect approaches to measure loneliness in later life. Res Aging (2011). 34(5):572–91. doi:10.1177/0164027511423258
51.World Health Organization. World report on ageing and health (2015). Available from: https://www.who.int/ageing/publications/world-report-2015/en/ Accessed 9 November 2019.
Keywords: loneliness, mortality, older adults, low- and middle-income countries, social ageing
Citation: Gao Q, Prina AM, Prince M, Acosta D, Luisa Sosa A, Guerra M, Huang Y, Jimenez-Velazquez IZ, Llibre Rodriguez JJ, Salas A, Williams JD, Liu Z, Acosta Castillo I and Mayston R (2021) Loneliness Among Older Adults in Latin America, China, and India: Prevalence, Correlates and Association With Mortality. Int J Public Health 66:604449. doi: 10.3389/ijph.2021.604449
Received: 09 September 2020; Accepted: 02 February 2021;
Published: 31 March 2021.
Edited by:
Nino Kuenzli, Swiss Tropical and Public Health Institute (Swiss TPH), SwitzerlandCopyright © 2021 Gao, Prina, Prince, Acosta, Luisa Sosa, Guerra, Huang, Jimenez-Velazquez, Llibre Rodriguez, Salas, Williams, Liu, Acosta Castillo and Mayston. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rosie Mayston, cm9zaWUubWF5c3RvbkBrY2wuYWMudWs=
 Qian Gao
Qian Gao A. Matthew Prina1
A. Matthew Prina1 Daisy Acosta
Daisy Acosta Ana Luisa Sosa
Ana Luisa Sosa Yueqin Huang
Yueqin Huang Ivonne Z. Jimenez-Velazquez
Ivonne Z. Jimenez-Velazquez Zhaorui Liu
Zhaorui Liu Isaac Acosta Castillo
Isaac Acosta Castillo