Abstract
Objectives: The main objectives of this study were to examine the prevalence of workplace violence (WPV), its associated factors and explore the experiences of healthcare workers.
Methods: A hospital-based cross-sectional study design used a nationally representative sample of 1,081 healthcare workers covering eight administrative divisions of Bangladesh. Logistic regression analysis was employed to estimate the adjusted effect of independent factors on WPV among healthcare workers.
Results: Of the participants, 43% (468) experienced some form of WPV. Of those, 84% reported experiencing nonphysical violence, and 16% experienced physical violence in the past year. About 65% of victims claimed no action was taken to investigate the incident, and 44% reported no consequence for perpetrators. Four factors: being married (AOR = 1.63; CI: 1.12–2.39); public sector healthcare worker (AOR = 2.74; CI:1.99–3.76); working in an emergency department (AOR = 2.30; CI:1.03–5.12); and undertaking shift work (AOR = 1.52; CI: 1.10–2.11) were found to be significantly associated with WPV. One-third of the participants were worried about violence in their workplace.
Conclusion: WPV is highly prevalent among healthcare workers in Bangladesh. Formal guidelines for reporting and managing WPV are urgently needed at the individual, hospital, and national levels.
Introduction
Workplace violence (WPV) encompasses both physical and nonphysical (verbal) violence. It is a growing public health concern among healthcare workers internationally, including in Bangladesh [1]. It is a key occupational hazard of healthcare workers. It is defined as any incident of a member of staff being abused, threatened, or assaulted on the grounds of their employment, including commuting to and from work, causing an implicit or explicit challenge to their safety, well-being, or health [2].
The World Health Organization (WHO) reported that violence in healthcare settings represents about a quarter of all violence in workplaces and that violence against healthcare workers is a global problem [3]. The WHO conducted a seven-country case study on WPV in the health sector and reported that more than 50% of responding workers experienced at least one incident of either physical or nonphysical violence in the preceding year: 37% in Portugal, 46% in Brazil, 54% in Thailand, 61% in South Africa, 67% in Australia, and 75% in Bulgaria [3]. A recent systematic review documented that the 12-months prevalence of any form of WPV was 61% globally among healthcare workers [4]. About 42% experienced nonphysical violence, for example, verbal abuse (57%), threats (32%), sexual advances (12%), while 24% reported physical violence. This review also indicated that 64% of Asian healthcare workers had experienced WPV: nonphysical 45% and physical 24% [4].
It is well known that violence occurs in all workplaces; however, healthcare workers are more prone to experience WPV than almost any other profession in both developed and developing countries [4, 5]. The prevalence of WPV among healthcare workers is high in Asian countries: 51% in Pakistan [6], 62% in China [7], and 63% in India [8]. These studies also estimated that verbal or nonphysical violence was more prevalent than physical violence among healthcare workers. In Bangladesh, violence against healthcare workers is not a new issue. An analysis of media reports suggests that 96% of reported violence cases were physical, 91% occurred in public health care settings, and 52% occurred in emergency departments [9]. Unfortunately, healthcare services in Bangladesh are experiencing severe shortages of skilled healthcare workers [10, 11].
Many studies have shown that nurses are more vulnerable than doctors and other healthcare workers [4, 6, 12] to WPV, while some studies found that doctors are most susceptible [8, 12]. Previous studies showed that a number of factors were associated with WPV in healthcare settings, including occupation, gender, age, marital status, healthcare level, healthcare sector, work schedule, and department [1, 2, 4–6, 8–10]. Most researchers reported that doctors [1, 4, 6], being male [4, 7], and younger age [2, 13] health workers have a higher risk of experiencing WPV. Additionally, healthcare workers who worked in the emergency department [1, 9, 10, 13], public hospital [1, 6, 9], tertiary healthcare facilities [1, 14], and shift work [4, 5, 13] were positively associated with WPV.
WPV has been associated with post-traumatic stress disorder symptoms such as being “super alert” and watchful, feeling chronic fatigue or being bothered by repeated memories of the incident, low performance, absenteeism and staff turnover, lower productivity, and motivation as well as professional dissatisfaction, leading to decreased quality of care for patients [3, 4]. WPV against healthcare workers has a devasting impact on victims’ psychological and social well-being [1, 4]. A significant portion of victims or those who witnessed WPV had some form of mental health consequence as a result. A recent study showed that around two-third of respondents had mental health problems after exposure to or witnessed violence [6]. After an episode of WPV, there are growing rates of missed workdays, burnout, job dissatisfaction, decreased productivity and ceasing employment [9, 13, 15]. In some cases of WPV, healthcare workers have protested to voice their opinion against offenders. This can lead to loss of workdays, reduced health services, and an increased burden on patients and the health care system [9, 13, 15].
Most reports on WPV and healthcare workers have appeared in the media through newspapers and electronic media in Bangladesh but without systematic research as to the actual prevalence and effects of WPV [9].
Therefore, this study sought to examine the prevalence of WPV, its associated factors and explore the experiences of healthcare workers. The study also aimed to examine preventive strategies and provide suggestions to policymakers.
Methods
Study Design and Participants
A hospital-based cross-sectional study of healthcare workers (doctors, nurses, others, e.g., midwives, laboratory technicians, administrative professionals) was conducted in primary, secondary, and tertiary level of healthcare settings, including public and private healthcare providers in eight administrative divisions of Bangladesh. The target population was healthcare workers who had patient contact. Personnel who met any of the following criteria were excluded: less than 1 year of work experience in the hospital, interns and trainees. Data were collected from November 2019 to March 2020.
Survey Procedures
Sampling was stratified by healthcare facility type at the political administration level. Specifically, primary care facilities provide healthcare at the sub-district level (Upazilla health complex and below); secondary healthcare settings are usually located at the district level, while tertiary healthcare settings consist of medical colleges, specialist hospitals, and national hospitals, healthcare institutes, etc. Convenient sampling of primary, secondary and tertiary healthcare facilities across eight divisions in both public and private sectors was undertaken.
A structured questionnaire was used to collect socio-demographic information, healthcare settings, healthcare sectors, details of violence experienced in the past 12 months, problems and impacts encountered by the violent episode, and preventive measures. Healthcare workers on duty were invited to complete the questionnaire, and these included doctors, nurses, midwives, and laboratory technicians who had patient contact in their daily practices. Before conducting the survey, the study objectives, aims, methods, and benefits of this study were explained, and participants gave their written approval or not before proceeding.
The questionnaire was based on the WHO instrumental survey tool, previously used in Australia, South Africa, Portugal, Bulgaria, and Thailand [12]. In this study, that questionnaire was slightly adapted. The questionnaire comprised three sections [1]: Socio-demographic information and professional background [2]; Experience of WPV in the last 12 months, types and the number of instances, rehabilitation assistance to victims and their satisfaction with the assistance, reasons for underreporting or not reporting violence, and victim responses to and consequences for perpetrators [3]; Participant witnessing of violence in the previous year, anxiety and knowledge of WPV and preventive strategies. After voluntary consenting to participate, each respondent completed an anonymous questionnaire and returned it to the data collector. Respondents’ names and addresses were not required. Based on this procedure, 1,081 valid responses were collected (78.3% correct response rate).
Operational Definition
Physical violence was defined as the application of force or action, including pinching, pushing, shoving, and spitting or kicking, with or without the use of weapons, as well as rape [3].
Non-physical violence was defined as verbal abuse, threats, bullying/mobbing, frightening action(s), and unwanted sexual advances [3].
Statistical Analysis
We calculated descriptive statistics for demographic characteristics and frequency of exposure to WPV. Frequency distributions were calculated (in percentage points) for physical and nonphysical violence experienced by personnel in each professional category. In the analytical exploration, binary logistic regression analysis was used to determine which demographic and professional characteristics (including gender, marital status, age, experience, profession, department, shift work involved) associated experiencing physical or nonphysical violence. Based on only separated explanatory variables, an unadjusted regression analysis was performed. In the final model (adjusted), potential explanatory variables were only considered if any label of the covariate was statistically significant with a p-value at 5% or less in the unadjusted model. Statistical analyses were performed with SPSS v.25.
Results
Demographic and Professional Characteristics of the Respondents
A total of 1,081 healthcare workers participated in this study from all regions of Bangladesh (Table 1). The mean age of participants was 30.83 years (SD: 6.75; min:20, max:67). The majority of participants were doctors (64.0%), female (52.3%), <35 years of age (71.5%) and married (60.2%). Over half of the participants had experienced less than 6 years (61.4%), worked in tertiary healthcare settings (72.7%), for the public health sector (55.0%), and in fixed shift (51.8%). The spatial distribution of respondents was even across the nation.
Table 1
| Participant characteristics | Number of participants (n) | Percentage of participants (%) |
|---|---|---|
| Profession | ||
| Doctors | 692 | 64.01 |
| Nurses | 285 | 26.36 |
| Other healthcare workers | 104 | 9.62 |
| Gender | ||
| Male | 516 | 47.73 |
| Female | 565 | 52.27 |
| Age | ||
| <35 years | 773 | 71.50 |
| 35–44 years | 261 | 24.14 |
| >44 years | 47 | 4.34 |
| Marital status | ||
| Married | 651 | 60.22 |
| Unmarried | 430 | 39.78 |
| Level of healthcare setting | ||
| Primary | 168 | 15.54 |
| Secondary | 127 | 11.75 |
| Tertiary | 786 | 72.71 |
| Type of healthcare sector | ||
| Public | 602 | 55.69 |
| Private | 479 | 44.31 |
| Years of experience | ||
| <6 years | 664 | 61.42 |
| 6–10 years | 211 | 19.51 |
| 11–15 years | 121 | 11.20 |
| 16–20 years | 44 | 4.07 |
| >20 years | 41 | 3.79 |
| Working department | ||
| General medicine | 148 | 13.69 |
| General surgery | 149 | 13.78 |
| Emergency | 169 | 15.63 |
| Intensive care | 54 | 5.00 |
| Pediatrics | 88 | 8.14 |
| Gynecology and obstetrics | 95 | 8.79 |
| Orthopedics | 49 | 4.53 |
| ENT (eye, nose and tongue) | 30 | 2.78 |
| Management | 36 | 3.33 |
| Other departments | 263 | 24.33 |
| Rotating shift work | ||
| Yes | 521 | 48.20 |
| No | 560 | 51.80 |
| Workplace location | ||
| Dhaka division | 258 | 23.86 |
| Chittagong division | 144 | 13.32 |
| Sylhet division | 100 | 9.25 |
| Khulna division | 120 | 11.10 |
| Rangpur division | 137 | 12.67 |
| Barisal division | 98 | 9.06 |
| Rajshahi division | 123 | 11.37 |
| Mymensingh division | 101 | 9.34 |
Participants’ demographic and professional characteristics, Bangladesh, 2020.
The prevalence of WPV varies by gender and profession (Figure 1). Overall, 468 (43.3%) incidents were reported, with 84.6% nonphysical and 15.4% physical. About 51.4% of doctors and 35.4% of nurses had exposure to some form of violence. Physicians were the most vulnerable to physical violence, while nurses were the most susceptible to nonphysical violence.
FIGURE 1
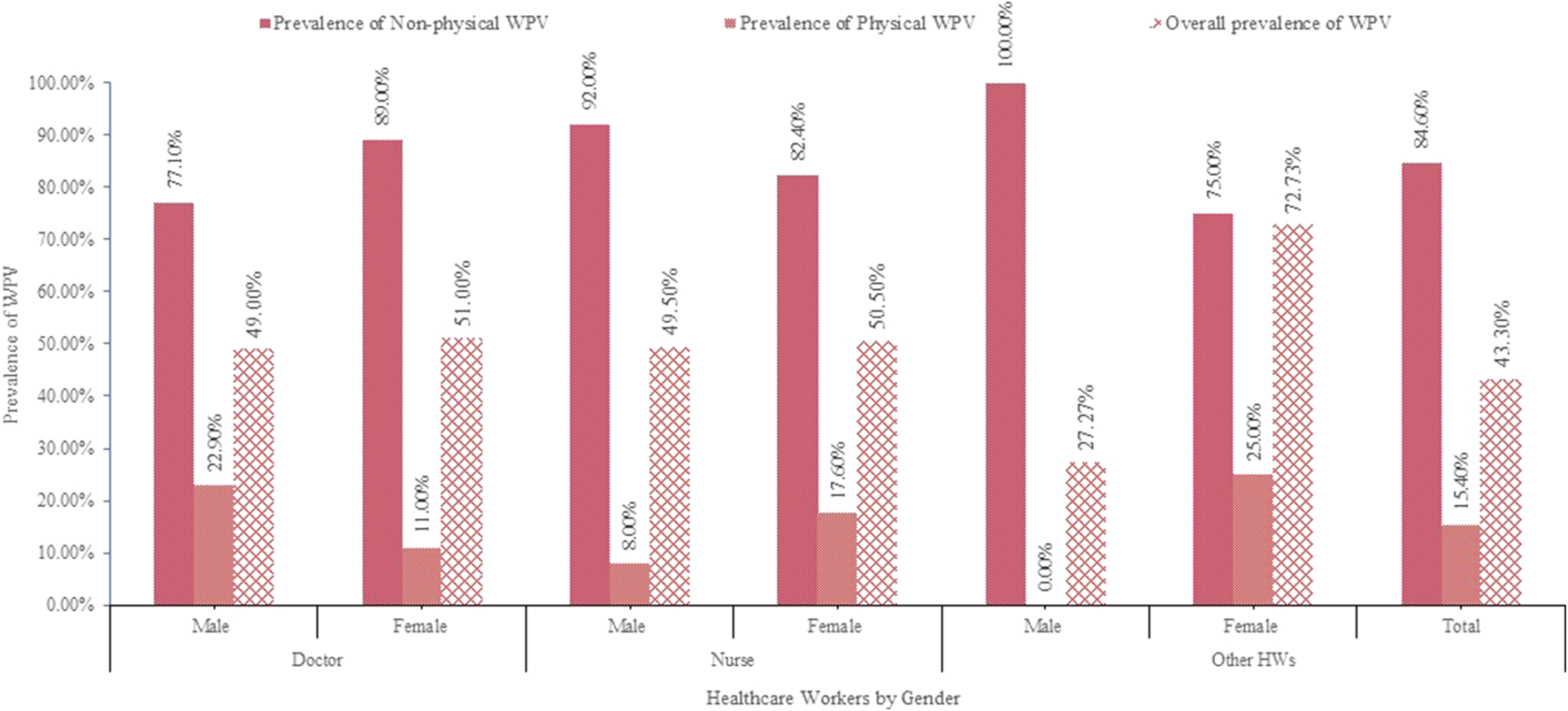
Prevalence of workplace violence (WPV) among healthcare workers, Bangladesh, 2020.
Associations Between Violence Exposure and Respondents’ Characteristics
Table 2 shows the outcome of the multiple logistic regression model, which was used to assess the predictive factors for WPV. It was found to be significantly associated with profession, marital status, health care sector, specialized department, and shift work (p < 0.05).
Table 2
| Participant characteristics | Prevalence of WPV | Unadjusted model | Adjusted model | ||
|---|---|---|---|---|---|
| OR | 95% CI | AOR | 95% CI | ||
| Profession | |||||
| Doctor | 356 (51.4) | 1.93 | 1.45–2.56 | 0.98 | 0.67–1.41 |
| Nurse (=ref) | 101 (35.4) | 1.00 | 1.00 | 1.00 | 1.00 |
| Other health workers | 11 (10.6) | 0.21 | 0.11–0.42 | 0.27 | 0.11–0.67 |
| Gender | |||||
| Female | 235 (42.6) | 0.93 | 0.73–1.18 | 0.99 | 0.74–1.33 |
| Male (=ref) | 233 (44.0) | 1.00 | 1.00 | 1.00 | 1.00 |
| Age | |||||
| <35 years | 274 (35.4) | 0.34 | 0.18–0.62 | 0.94 | 0.16–5.39 |
| 35–44 years | 165 (63.2) | 1.07 | 0.56–2.02 | 1.33 | 0.26–6.84 |
| >44 years (=ref) | 29 (61.7) | 1.00 | 1.00 | 1.00 | 1.00 |
| Marital status | |||||
| Married | 331 (50.8) | 2.21 | 1.71–2.85 | 1.63 | 1.12–2.39 |
| Unmarried (=ref) | 137 (31.9) | 1.00 | 1.00 | 1.00 | 1.00 |
| Healthcare setting | |||||
| Primary | 55 (32.7) | 0.59 | 0.42–0.84 | 0.84 | 0.50–1.39 |
| Secondary | 59 (46.5) | 1.06 | 0.73–1.54 | 0.96 | 0.60–1.53 |
| Tertiary (=ref) | 354 (45.0) | 1.00 | 1.00 | 1.00 | 1.00 |
| Healthcare sector | |||||
| Public | 325 (54.0) | 2.75 | 2.14–3.55 | 2.74 | 1.99–3.76 |
| Private | 143 (29.9) | 1.00 | 1.00 | 1.00 | 1.00 |
| Years of experience | |||||
| <6 years | 205 (30.9) | 0.26 | 0.13–0.49 | 0.50 | 0.08–3.23 |
| 6–10 years | 124 (58.8) | 0.82 | 0.41–1.64 | 0.84 | 0.14–5.15 |
| 11–15 years | 86 (71.1) | 1.42 | 0.67–2.99 | 1.06 | 0.17–6.50 |
| 16–20 years | 27 (61.4) | 0.91 | 0.38–2.20 | 0.62 | 0.12–3.08 |
| >20 years (=ref) | 26 (63.4) | 1.00 | 1.00 | 1.00 | 1.00 |
| Working department | |||||
| General medicine | 60 (40.5) | 0.61 | 0.29–1.26 | 0.64 | 0.29–1.41 |
| General surgery | 76 (51.0) | 0.93 | 0.45–1.93 | 1.22 | 0.55–2.74 |
| Emergency | 123 (72.8) | 2.39 | 1.14–4.99 | 2.30 | 1.03–5.12 |
| Intensive care | 26 (48.1) | 0.83 | 0.35–1.93 | 0.85 | 0.33–2.15 |
| Pediatrics | 42 (47.7) | 0.82 | 0.37–1.77 | 0.78 | 0.34–1.80 |
| Gyne and obstetrics | 37 (38.9) | 0.57 | 0.26–1.23 | 0.56 | 0.24–1.30 |
| Orthopedics | 22 (44.9) | 0.73 | 0.30–1.72 | 0.59 | 0.22–1.48 |
| E.N.T. department | 14 (46.7) | 0.78 | 0.29–2.06 | 0.76 | 0.26–1.98 |
| Other departments | 49 (18.6) | 0.20 | 0.09–0.42 | 0.37 | 0.17–0.79 |
| Management (=ref) | 19 (52.8) | 1.00 | 1.00 | 1.00 | 1.00 |
| Rotating shift work | |||||
| Yes | 290 (55.7) | 2.69 | (2.10–3.45) | 1.52 | 1.10–2.11 |
| No (=ref) | 178 (31.8) | 1.00 | 1.00 | 1.00 | 1.00 |
| Hosmer-Lesmeshow statistics (p value) | 17.42 (p = 0.26) | ||||
Multivariate adjusted and unadjusted odds for respondents’ exposure to violence, Bangladesh, 2020.
Compared to nurses, violence among doctors was higher (51.4%). The prevalence of WPV was significantly lower among other healthcare workers (AOR = 0.27; CI: 0.11–0.67). Participants who were married experienced a higher prevalence of WPV compared to those never married (AOR = 1.63; CI: 1.11–2.38). Participants from the public sector experienced 2.73 times higher WPV than their private-sector colleagues (AOR = 2.73; CI: 1.99–3.76).
Healthcare workers in emergency departments (AOR = 2.30; CI: 1.03–5.12) were more likely to have experienced WPV than those who worked in other departments. WPV was also higher among healthcare workers who were shift workers (AOR = 1.52; CI: 1.10–2.11).
Perpetrators and Consequences
Regarding perpetrators, family members or relatives of the patients were the main perpetrators (73.1%), while 29.1% of cases involved the patient. Approximately 14.3% of victims reported being injured due to violence, while 22.4% had to leave work after being subjected to violence. Approximately 65% of victims claimed no action was taken to investigate the incident and 44.0% reported no consequences for the perpetrator(s) (Table 3).
Table 3
| Variables | Number | Percentage |
|---|---|---|
| Perpetrators | ||
| Patient | 136 | 29.10 |
| Relatives of the patient | 342 | 73.10 |
| Staff member | 27 | 5.80 |
| Supervisor or management | 44 | 9.40 |
| General Public | 54 | 11.50 |
| Injuries caused by violence | ||
| Yes | 67 | 14.30 |
| No | 401 | 85.70 |
| After being a victim, take time off from work | ||
| Yes | 105 | 22.40 |
| No | 363 | 77.60 |
| Action was taken to investigate the incident | ||
| Yes | 81 | 17.30 |
| No | 306 | 65.40 |
| Don’t know | 81 | 17.30 |
| Consequences for the perpetrator | ||
| None | 206 | 44.00 |
| Verbal warning | 79 | 16.90 |
| Care discontinued | 16 | 3.40 |
| Reported to police | 16 | 3.40 |
| Aggressor prosecuted | 9 | 1.90 |
| Do not know | 142 | 30.30 |
| Victims respond to the incident | ||
| Yes | 128 | 27.40 |
| No | 340 | 72.60 |
| Incident was preventable | ||
| Yes | 282 | 60.30 |
| No | 186 | 39.70 |
| Supports from employer | ||
| Yes | 94 | 20.10 |
| No | 374 | 79.90 |
| Satisfaction with the way the situation was handled | ||
| Yes | 95 | 20.30 |
| No | 373 | 79.70 |
| Reason for not reporting or talking about the incident | ||
| It was not important | 68 | 14.50 |
| Felt ashamed | 50 | 10.70 |
| Felt guilty | 22 | 4.70 |
| Afraid of negative consequence | 88 | 18.80 |
| Fear of being fire from job | 58 | 12.40 |
| Did not know who to report | 77 | 16.50 |
| Others | 105 | 22.40 |
| Worried about violence in the current workplace | ||
| Not worried at all | 265 | 24.5 |
| A little | 300 | 27.8 |
| Worried | 244 | 22.6 |
| Very worried | 272 | 25.2 |
| Procedures for the reporting of violence in the workplace | ||
| Yes | 422 | 39.0 |
| No | 265 | 24.5 |
| Don’t know | 394 | 36.4 |
| Participated in any violence prevention training program | ||
| Yes | 251 | 23.2 |
| No | 830 | 76.8 |
| Existing WPV prevention and control policies in the workplace | ||
| Yes | 118 | 10.9 |
| No | 382 | 35.3 |
| Don’t know | 581 | 53.7 |
Distribution of study participants exposed to workplace violence, Bangladesh, 2020.
Reactions of Victims and Underreporting of WPV
Most of the victims (72.6%) stated that they did not react to the incident, while 60.3% believed it could have been prevented. Most victims (79.9%) claimed that their employer did nothing when the violence was reported to them, and 79.7% were not satisfied with the manner in which the situation was handled (Table 3).
WPV victims disclosed various types of reasons for not reporting incidents to the authorities. About 14.5% of victims thought it was unimportant, 16.5% said they did not know whom to report to, 18.8% were afraid of negative consequences, 10.7% felt ashamed, and 12.4% were afraid of being fired from their job. About 24.4% of participants were not worried about violence in their current workplace, while 27.8% were a little worried, 22.6% were worried, and 25.2% were very worried (Table 3).
Knowledge of preventive strategies and suggestions to prevent WPV About 24.5% of victims claimed no procedures for reporting the violent incidences, and 36.4% stated they had no idea about the process for reporting violence at their workplace. Participants were asked about any training or workshops on WPV they had undertaken, and 76.8% replied that they had not taken part in any training or workshop to deal with WPV. Over half of respondents (53.7%) stated no existing WPV prevention and control policies in their workplace (Table 3).
Participants were also asked about measures that could be taken to prevent violence. All participants could mark more than one choice. Measures that could be taken to avoid the violence include security measures 67.2% (727), improving surroundings 59.4% (642), increased staff members 52.2% (565), and patient protocol 50.3% (544). They also suggested that training programs, reduced time working alone, shift changes, restricting public access, and restricting money exchange in hospitals could also be effective (Figure 2).
FIGURE 2
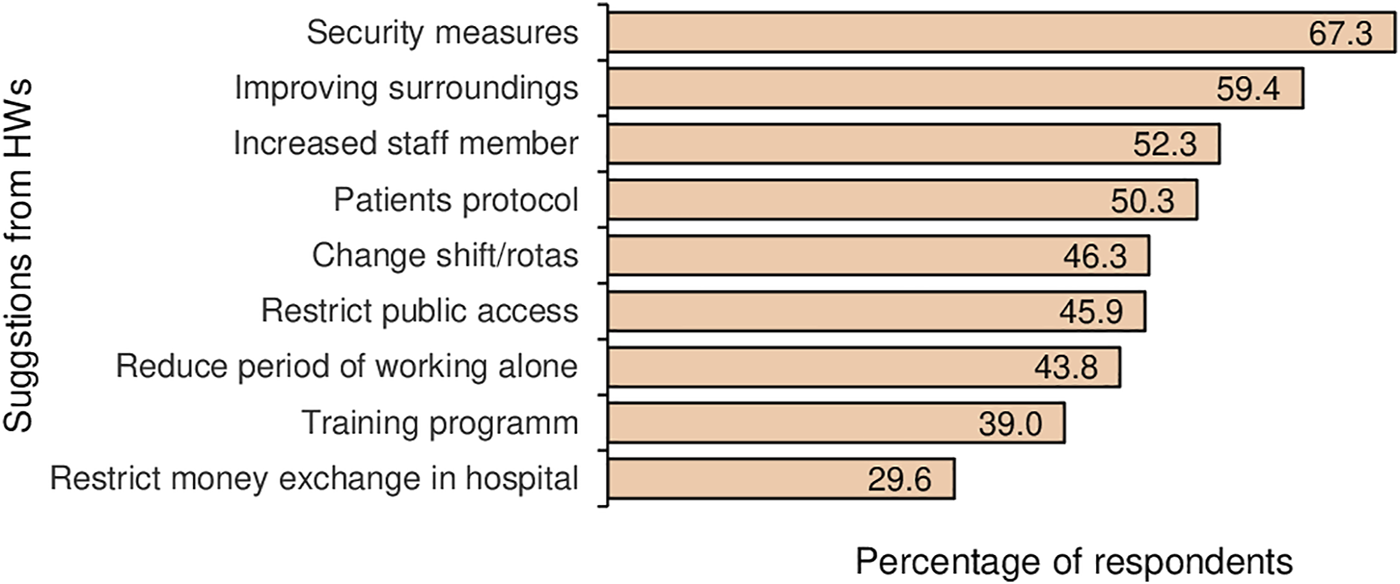
Suggestions from healthcare workers (HW) to prevent workplace violence (multiple responses), Bangladesh, 2020.
Discussion
This study investigated workplace violence experiences among healthcare workers (doctors, nurses, midwives, medical technologists, administrative staff) in Bangladesh and its characteristics. The analysis revealed the overall prevalence of WPV and differences in prevalence among various categories of healthcare workers. Moreover, the distribution of physical and nonphysical violence, associated factors, and potential preventive strategies was analyzed.
This study obtained a 43.3% prevalence of WPV among healthcare workers, of which 84.6% were non-physical, and the remaining 15.4% was physical. The prevalence is lower than a study conducted in China (49.2%) [17] but higher than in India (40.8%) [18]. A Turkish study of doctors identified a very high 78.1% prevalence of WPV in the emergency department [16]. The current study has also revealed that respondents from the emergency department (72.8%), followed by management (52.8%) and general surgery (51%), were more likely to have experienced violence than those who worked in other departments. There have been increasing workplace violence trends, as previously reported that in Bangladesh, 91% of violence took place in public healthcare settings [9]. Studies conducted worldwide identified quite diverse prevalence rates among the various types of health care professionals and at multiple levels (primary, secondary, tertiary) [14, 19, 20]. In this study, a higher prevalence of WPV among doctors compared to nurses was observed. However, WPV was very low (10.6%) among other healthcare workers. The prevalence was also relatively low in primary health care settings compared to secondary and tertiary levels.
Doctors in an emergency, psychiatrists, and those involved with primary care are at increased risk of violent acts from patients and families. Emergency departments, intensive care units, and post-surgical wards are the most common settings for violence [19, 20]. Working in an emergency department with a high patient admission rate increases the probability of experiencing WPV [16]. There were statistically significant differences in the experience of violence who worked at public and private hospitals. A study conducted in Palestine showed a tendency for those who worked in public hospitals to be more likely to experience violence [21]. Further, respondents who were shift workers were four times more likely to have experienced violence than those who did not work shifts [22].
There are often difficulties with relations between healthcare workers and their patients in Bangladesh, as multiple newspaper reports collated and published recently can attest [23]. Most perpetrators of violence were relatives of the patient. An Indian study also identified similar findings as perpetrators were visitors/relatives (48%), patients (38%), and co-workers (14%) [21].
Non-reporting of violence is a concerning issue, mainly due to the lack of policy or procedure and management support, having previous experience of no action taken, and fear of the consequences. The results identified not knowing whom to report to as the main reason behind non-reporting. The majority of the victims took no action to investigate the incidents, and 36.6% had no idea about the consequences for the perpetrator(s).
The study results confirm that among the suggested measures, security measures were the most commonly implemented. However, these measures were reactive rather than proactive and tackled a particular risk (physical violence) rather than WPV as a whole. In light of international and national experiences, it is only with comprehensive preventive measures and penalties that actions against WPV at hospitals can be practical.
As outlined in the international labor organization (ILO) convention (No. 190) and recommendation (No. 206), “Governments should adopt legislation requiring employers to secure adequate protection against workplace violence and harassment.” [24]. However, no national guidelines in Bangladesh ensure employers’ legal responsibility to provide a safe, decent and healthy working environment for employees, where protection of their legitimate rights is enforced. The interests of health workers and, in particular, their safety is not being prioritized by specific government legislation.
The outlined WPV preventive measures are widely accepted as comprehensive measures to address workplace the risk factors of WPV. Therefore, the following are suggestions for wide measures to combat WPV in hospitals in Bangladesh. First, create a positive culture to combat violence. To create a harmonious doctor-patient relationship, respect, tolerance, gender sensitivity, equality, collaboration, and care should be practiced, and no form of WPV should be tolerated. Second, organizational interventions should be conducted whereby hospitals need to invest in human resource development. Improving staff or patient rations to reduce staff shortages will minimize time pressure on health workers. Effective organization of workloads can reduce the number of consecutive night shifts and the long working hours experienced.
Third, implement interventions to optimize service delivery to reduce waiting times, design comfortable and convenient waiting areas, and design escape doors for high-risk departments (such as emergency) staff. It is crucial to limiting public access, including security checks on visitors, and provide safe areas for staff (such as changing rooms). Fourth, hospitals should be required to provide victims with medical treatment, psychological counseling, and financial compensation, while perpetrators should be punished under the law. Fifth, develop and introduce practical measures for prevention and control, such as measuring the prevalence of violence, the impact of violence, and undertaking risk assessments.
Strengths and Limitations
This survey is the first comprehensive study of WPV against healthcare workers and revealed the WPV situation in healthcare settings in Bangladesh. In this study, relatively a large sample size was obtained, considering the total number of healthcare workers in Bangladesh. The study results can contribute to developing appropriate policy and strategies on WPV against healthcare workers and serve as the basis for future research in the country.
This study has several limitations. First, this study was completed in response to an open invitation; thus, it might have been completed mainly by healthcare workers who had been subjected to violence in the past and therefore are more sensitive to this issue. Data were collected retrospectively; these methods rely on the respondents’ ability to recall events in the past year, which could result in recall bias. Second, a convenience sampling design was used in this study, so the results cannot be generalized. Finally, the survey was not tested and validated before this study.
Conclusion
This study has outlined the prevalence of WPV among healthcare workers in Bangladesh, and the results indicate that these healthcare workers are vulnerable to WPV. Several potential associated factors of WPV, such as profession, marital status, healthcare sector, specialized department, and shift work was observed. Some critical factors, such as the reluctant attitudes of employers and employees regarding WPV, which include underreporting by employees, lack of knowledge among healthcare workers, low job security, and inefficient action by authorities, are some of the primary reasons behind the burden of WPV. Considering our findings, this issue cannot be ignored, especially from the point of view of occupational health and safety. To reduce WPV and create safe working environments, we recommend developing preventive safety policies, procedures, and prevention training. Further research is needed to understand how to reduce WPV against healthcare workers.
Statements
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board (IRB) at North South University, Dhaka-1229, Bangladesh (2020/OR-NSU/IRB-No.0801). The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
Conceptualized the study: MS; Contributed data extraction and analyses: MS under the guidance of RAM. Result interpretation: MS under the guidance of RAM. Prepared the first draft: MS, JG, MMA, TA and RAM. Contributed during the conceptualization and interpretation of results and substantial revision: MS, JG, MMA, MDHH, TA, SKC, FMM, and RAM. Revised and finalized the final manuscript: MS, JG, MMA, MDHH, TA, SKC, FMM, and RAM. All authors read and approved the final version of the manuscript.
Acknowledgments
We would like to thank everyone who took part in this survey. We also want to thank the data collectors and hospital authorities for their assistance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Ma J Chen X Zheng Q Zhang Y Ming Z Wang D et al Serious Workplace Violence against Healthcare Providers in China between 2004 and 2018. Front Public Health (2021) 8:574765. 10.3389/fpubh.2020.574765
2.
Kobayashi Y Oe M Ishida T Matsuoka M Chiba H Uchimura N . Workplace Violence and its Effects on Burnout and Secondary Traumatic Stress Among Mental Healthcare Nurses in Japan. Int J Environ Res Public Health (2020) 17(8):2747. 10.3390/ijerph17082747
3.
Di Martineo V . Workplace Violence in the Health Sector Country Case Studies Brazil, Bulgaria, Lebanon, Portugal, South Africa, Thailand and an Additional Australian Study. Synth Rep (2009) 2009:1–49. Available from: https://www.who.int/violence_injury_prevention/violence/activities/workplace/WVsynthesisreport.pdf?ua=1 (Accessed August 8, 2021).
4.
Liu J Gan Y Jiang H Li L Dwyer R Lu K et al Prevalence of Workplace Violence against Healthcare Workers: A Systematic Review and Meta-Analysis. Occup Environ Med (2019) 76:927–37. 10.1136/oemed-2019-105849
5.
Needham I Mckenna K . Workplace Violence in the Health Sector. Proc First Int Conf Work Violence Heal Sect - Together, Create a Safe Work Environ (2008). p. 383. Available from: http://www.mtpinnacle.com/pdfs/Boek_Workplace_Violence.pdf (Accessed August 8, 2021).
6.
Khan MN Haq ZU Khan M Wali S Baddia F Rasul S et al Prevalence and Determinants of Violence against Health Care in the Metropolitan City of Peshawar: a Cross Sectional Study. BMC Public Health (2021) 21(1):330. 10.1186/s12889-021-10243-8
7.
Lu L Dong M Wang S-B Zhang L Ng CH Ungvari GS et al Prevalence of Workplace Violence against Health-Care Professionals in China: A Comprehensive Meta-Analysis of Observational Surveys. Trauma, Violence, & Abuse (2020) 21(3):498–509. 10.1177/1524838018774429
8.
Hossain MM Sharma R Tasnim S Al Kibria GM Sultana A Saxena T . Prevalence, Characteristics, and Associated Factors of Workplace Violence against Healthcare Professionals in India: A Systematic Review and Meta-Analysis. Evid Based Psychosocial Health (2020). 10.1101/2020.01.01.20016295
9.
Hasan MI Hassan MZ Bulbul MMI Joarder T Chisti MJ . Iceberg of Workplace Violence in Health Sector of Bangladesh. BMC Res Notes (2018) 11(1):702. 10.1186/s13104-018-3795-6
10.
Hossain R . Current Status of Health Sector in Bangladesh. Bangladesh Med J (2016) 44(1):46–50. 10.3329/bmj.v44i1.26356
11.
Global Health Workforce Alliance. Health Workers for All and All for Health Workers: An Agenda for Global Action (2008). p. 1–8. Available from: https://www.who.int/workforcealliance/countries/bgd/en/(Accessed August 8, 2021).
12.
Di Martino V . Country Case Studies: Brazil, Bulgaria, Lebanon, Portugal, South Africa, Thailand and an Additional Australian Study (2002). Available from: https://www.who.int/violence_injury_prevention/violence/activities/workplace/WVsynthesisreport.pdf?ua=1 (Accessed August 8, 2021).
13.
Kumari A Kaur T Ranjan P Chopra S Sarkar S Baitha U . Workplace Violence against Doctors: Characteristics, Risk Factors, and Mitigation Strategies. J Postgrad Med (2020) 66(3):149–54. 10.4103/jpgm.JPGM_96_20
14.
Li Y-L Li R-Q Qiu D Xiao S-Y . Prevalence of Workplace Physical Violence against Health Care Professionals by Patients and Visitors: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health (2020) 17(1):299. 10.3390/IJERPH17010299
15.
Sun T Gao L Li F Shi Y Xie F Wang J et al Workplace Violence, Psychological Stress, Sleep Quality and Subjective Health in Chinese Doctors: a Large Cross-Sectional Study. BMJ Open (2017) 7(12):e017182. 10.1136/bmjopen-2017-017182
16.
Bayram B Çetin M Çolak Oray N Can İÖ . Workplace Violence against Physicians in Turkey's Emergency Departments: a Cross-Sectional Survey. BMJ Open (2017) 7(6):e013568. 10.1136/bmjopen-2016-013568
17.
Jia H Fang H Chen R Jiao M Wei L Zhang G et al Workplace Violence against Healthcare Professionals in a Multiethnic Area: a Cross-Sectional Study in Southwest China. BMJ Open (2020) 10(9):e037464. 10.1136/bmjopen-2020-037464
18.
Lindquist B Koval K Mahadevan A Gennosa C Leggio W Niknam K et al Workplace Violence Among Prehospital Care Providers in India: A Cross-Sectional Study. BMJ Open (2019) 9(11):e033404. 10.1136/bmjopen-2019-033404
19.
Vento S Cainelli F Vallone A . Violence against Healthcare Workers: A Worldwide Phenomenon with Serious Consequences. Front Public Health (2020) 8:541. 10.3389/FPUBH.2020.570459
20.
Tian Y Yue Y Wang J Luo T Li Y Zhou J . Workplace Violence against Hospital Healthcare Workers in China: a National WeChat-Based Survey. BMC Public Health (2020) 20(1):1–8. 10.1186/S12889-020-08708-3
21.
Kitaneh M Hamdan M . Workplace Violence against Physicians and Nurses in Palestinian Public Hospitals: a Cross-Sectional Study. BMC Health Serv Res (2012) 12(1):1–9. 10.1186/1472-6963-12-469
22.
Campbell JC Messing JT Kub J Agnew J Fitzgerald S Fowler B et al Workplace Violence. J Occup Environ Med (2011) 53(1):82–9. 10.1097/JOM.0b013e3182028d55
23.
Hasan MI Hassan MZ Bulbul MMI Joarder T Chisti MJ . Iceberg of Workplace Violence in Health Sector of Bangladesh. BMC Res Notes (2018) 11(1):1–6. 10.1186/s13104-018-3795-6
24.
International Labour Organization. New International Labour Standard to Combat Violence, Harassment, at Work Agreed (2019). Available from: https://www.ilo.org/ilc/ILCSessions/108/media-centre/news/WCMS_711321/lang--en/index.htm (Accessed August 8, 2021).
Summary
Keywords
healthcare workers, prevention, physical violence, non-physical violence, workplace of violence
Citation
Shahjalal M, Gow J, Alam MM, Ahmed T, Chakma SK, Mohsin FM, Hawlader MDH and Mahumud RA (2021) Workplace Violence Among Health Care Professionals in Public and Private Health Facilities in Bangladesh. Int J Public Health 66:1604396. doi: 10.3389/ijph.2021.1604396
Received
09 August 2021
Accepted
10 December 2021
Published
31 December 2021
Volume
66 - 2021
Edited by
Nino Kuenzli, Swiss Tropical and Public Health Institute (Swiss TPH), Switzerland
Reviewed by
Andrew Gibbs, South African Medical Research Council, South Africa
Jihene Sahli, University of Sousse, Tunisia
Updates
Copyright
© 2021 Shahjalal, Gow, Alam, Ahmed, Chakma, Mohsin, Hawlader and Mahumud.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Md. Shahjalal, md.shahjalal3@northsouth.edu
This Original Article is part of the IJPH Special Issue “Health in All Sustainable Development Goals”
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.