- 1School of Public Health, University of Alberta, Edmonton, AB, Canada
- 2Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
- 3MAP Centre for Urban Health Solutions, Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, ON, Canada
Objectives: Children’s mental health and wellbeing declined during the first COVID-19 lockdown (Spring 2020), particularly among those from disadvantaged settings. We compared mental health and wellbeing of school-aged children observed pre-pandemic in 2018 and after the first lockdown was lifted and schools reopened in Fall 2020.
Methods: In 2018, we surveyed 476 grade 4–6 students (9–12 years old) from 11 schools in socioeconomically disadvantaged communities in Northern Canada that participate in a school-based health promotion program targeting healthy lifestyle behaviours and mental wellbeing. In November-December 2020, we surveyed 467 grade 4–6 students in the same schools. The 12 questions in the mental health and wellbeing domain were grouped based on correlation and examined using multivariable logistic regression.
Results: There were no notable changes pre-pandemic vs. post-lockdown in responses to each of the 12 questions or any of the sub-groupings.
Conclusion: Supporting schools to implement health promotion programs may help mitigate the impact of the pandemic on children’s mental health and wellbeing. The findings align with recent calls for schools to remain open as long as possible during the pandemic response.
Introduction
On March 11, 2020 the World Health Organization declared the COVID-19 pandemic. While implemented public health measures were critical to combat the viral spread, 1.6 billion children have been affected by school closures, cancellations or modification of organized sport and recreation activities, and the enforcement of physical distancing and stay-at-home orders [1]. Although school-aged children are at a considerably lower risk of severe COVID-19 illness [2], early reports indicate that the pandemic–through associated public health measures–jeopardized children’s mental health and wellbeing during the first lockdown in Spring 2020 [3]. The burden of mental illness among children was high even before the pandemic, with as many as 20% of youth living with a mental disorder in Canada [4]. The pandemic added myriad stressors that impact children’s mental health and wellbeing (e.g., fear of contracting or having loved ones contract COVID-19, feelings of loneliness and hopelessness, and the inability to seek comfort from extended family members and friends) [5]. Among 385 Canadian children and adolescents, 67–70% experienced deterioration in at least one mental health domain during the first lockdown, particularly among those with pre-existing mental health problems [6], while the rates of mental disorders in 5–16 year old children in the United Kingdom increased from 11% in 2017 to 16% in July 2020 [7]. The risk for poor mental health and wellbeing is even higher for children from socioeconomically disadvantaged settings who may experience additional stressors such as household food insecurity, parental loss of jobs or income [8], and disruptive family dynamics [9], leaving children even more vulnerable when schools are closed as part of the COVID-19 response.
Schools play a critical role in the social development of children and, under normal circumstances, schools are where children spend the majority of their waking hours, where families connect before and after school hours, and are an integral setting of social support in the community. For children from vulnerable settings, schools can also act as a “protective layer” through the delivery of school-based programming, including nutrition programs and mental health support [10]. In case of school closure, the daily routine and social interactions are severely disrupted, leaving children at a potentially higher risk of loneliness and mental health problems [11]. Emerging evidence reports on the increase in depression symptoms and psychological distress in general populations of school-aged children during the first lockdown in Spring 2020 [3, 5, 6]. An important and timely question is whether the mental health and wellbeing of school-aged children resemble the pre-pandemic levels when children return to school, particularly among children from socioeconomically disadvantaged areas. In 11 rural and remote Northern communities in Canada, we compared mental health and wellbeing of school-aged children observed pre-pandemic in 2018 and after the first lockdown was lifted and schools reopened in Fall 2020.
Methods
In the Spring of 2018, we surveyed 9–12 year old students in grade 4–6 in 15 schools in rural and remote Northern communities in Canada. All schools participate in APPLE Schools (A Project Promoting healthy Living for Everyone in schools)—an innovative, internationally recognized, not-for-profit health program that promotes healthy lifestyle behaviours and mental wellbeing in schools located in socioeconomically disadvantaged communities [12]. Grounded in a Comprehensive Schools Health approach [13], APPLE Schools program helps to transform the school’s culture to “make the healthy choice the easy choice” [14–18]. From November 4 to December 9, 2020, we repeated this survey among grade 4–6 students in 11 of these 15 schools: one school declined participation and three other schools were closed due to COVID-19 outbreaks during the data collection. Eight schools are located in rural (<1,000 people) and three in small population centres (1,000–29,999 people) (Table 1). According to the 2016 Canadian Census data, population in these communities ranged from 414 to 14,961. Of the rural schools, two are located on an Indian reserve or settlement, and one community is “fly-in” only. Data were collected in school during regular class time. Students logged into the online survey portal on their Chromebooks, using a unique username and password that was assigned to them. Data collection shifted from the in-person mode in 2018 (trained research assistants travelled to schools to administer the surveys) to the online mode in accordance with the COVID-19 protocols (trained research assistants connected to each classroom through Zoom to prompt the survey questions that were projected on the whiteboard in the classroom). A total of 476 and 467 students completed the survey, with the participation rates of 71.5 and 78% in 2018 and 2020, respectively. All students provided assent and their parents/guardians provided active-information passive-permission consent. The Health Research Ethics Board of the University of Alberta (Pro00061528) and participating school boards approved all the procedures.
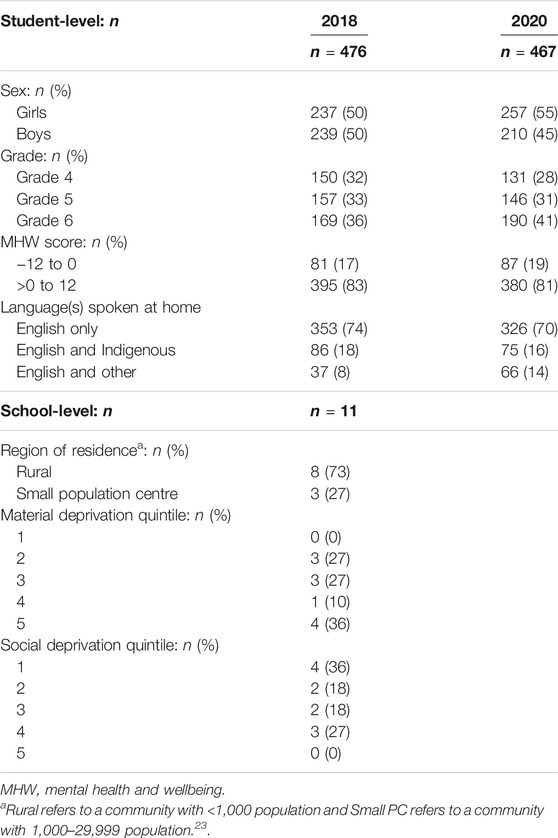
TABLE 1. Characteristics of 9–12-year-old students before the pandemic and after the first lockdown and school reopening, Canada, 2018–2020.
As part of the pandemic response, all in-school learning was suspended for K-12 schools on March 16 in Northwest Territories, March 17 in Alberta, and March 23 in Manitoba. Although school buildings were closed, online learning continued until June 2020. Since all 11 schools fall under the jurisdiction of respective provincial and territorial governments, they re-opened in September 2020, with enhanced public health measures to prevent viral transmission in schools, including mandatory masking and physical distancing, small group cohorting, and curricula adaptations (e.g., physical education classes).
As part of a survey on lifestyle behaviours (e.g., physical activity, sedentary behaviour, sleep, healthy eating), students completed a series of 12 questions in the domain of mental health and wellbeing suitable for grade 4–6 students, derived from population survey instruments [19–22]. These included five negatively phrased items: I worry a lot; I feel unhappy or sad; I have trouble paying attention; I have trouble enjoying myself; and I am in trouble with my teacher(s). Seven positively phrased items were: My future looks good to me; I have someone I trust to go to for advice; I do well in my schoolwork; I feel like I have many friends; I feel like I belong at schools; I like myself; and I like the way I look. For ease of interpretation, we centred the distribution around zero: response options (“never or almost never,” “sometimes,” and “often or almost always”) were assigned a score of “−1”, “0” and “1” for positively stated items and reverse coded for negatively stated items. The items were summed to create a cumulative score, ranging from −12 to +12, with higher values indicating better mental health and wellbeing (henceforward referred to as MHW score). Finally, the score was dichotomized using “0” as the cut-off value, with values above 0 representing better mental health and wellbeing, and between −12 and 0 (inclusive) worse mental health and wellbeing.
Students self-reported their sex (girl vs. boy). Covariates included student’s grade, region of residence, and quintiles of area-based social and material deprivation indices. Region of residence was defined according to Statistics Canada classification as rural (<1,000 people) or small population centre (1,000–29,999 people) [23]. Social and material deprivation indices were derived from 2016 Canada Census data based on postal codes, with higher quintiles indicating higher deprivation (detailed procedures are available elsewhere [24]). The polychoric correlation between the quintiles of these indices (−0.26) was estimated to rule out concerns about collinearity. To ensure sufficient number of students and schools in each category, quintiles were combined to create a binary variable indicating lower vs. higher deprivation (1–3 vs. 4-5 for material deprivation and 1–2 vs. 3-5 for social deprivation for material deprivation).
Differences in responses to each of the 12 items in 2018 and 2020 were examined using a chi-square test with a Bonferroni correction (p-values below 0.004 were considered statistically significant), separately for girls and boys. In all other analyses p-values below 0.05 were considered statistically significant. A student’s t-test was used to examine differences in the cumulative scores in 2018 and 2020. The distribution of the scores in 2018 and 2020 was depicted using histograms and Kernel density plots. A multivariable logistic regression model was applied to compare the odds of having worse vs. better mental health and wellbeing in 2020 compared to 2018 after adjustment for covariates.
To acknowledge that certain clusters of items may reveal temporal changes in mental health and wellbeing that are not necessarily captured in the MHW score, gender-stratified exploratory factor analysis with varimax (orthogonal) rotation was employed on the 2018 observations to extract latent factors that maximized the explained variance. Following examination of the scree plot and based on the Kaiser criterion (eigenvalue >1), three clusters were identified separately for girls and boys. Factor scores were then calculated using the Bartlett’s test of sphericity and dichotomized with scores greater than 0 representing doing better and those 0 and below doing worse in each of these clusters. Logistic regression was applied to estimate the odds of doing worse in 2020 compared to 2018 for the sub-grouping identified in each of the three clusters. For the missing values, we performed multiple imputation using multivariate imputation by chain equations (MICE) [25]. Approximately 91% of students provided responses to 12 items, and approximately 97% completed at least ten of the items. Three and 16 students who did not respond to six or more items in 2018 and 2020, respectively, were excluded from analyses. To acknowledge the nested data structure (students within schools), mixed effects models with a school-level random effect were tested. However, since the intra-class correlation appeared low (ranging between 0 and 0.02 for all models), we applied fixed effects regression models rather than mixed effects models as per established recommendations [26]. Analyses were conducted in R 4.0.2 software (GNU General Public License).
Results
Table 1 shows the characteristics of the participants and school communities before the pandemic (2018) and after the first lockdown was lifted (2020). While an equal number of girls and boys participated in 2018 survey, there were slightly more girls (56%) participating in the 2020 survey. Compared to the 2018 survey before the pandemic, fewer grade four (27 vs. 32%) and more grade six (41 vs. 36%) students participated in the survey during the pandemic. Four and three schools are located in the most materially and socially deprived areas, respectively.
Table 2 depicts the student responses to the 12 items in 2018 and 2020. For none of the items, the differences between 2018 and 2020 were either substantial or statistically significant. Slightly more boys responded “often or almost always” to two items: “I feel like I belong in school” (53% in 2020 vs. 45% in 2018) and “I have trouble enjoying myself” (58% in 2020 vs. 49% in 2018). The differences in girls’ responses were less pronounced.
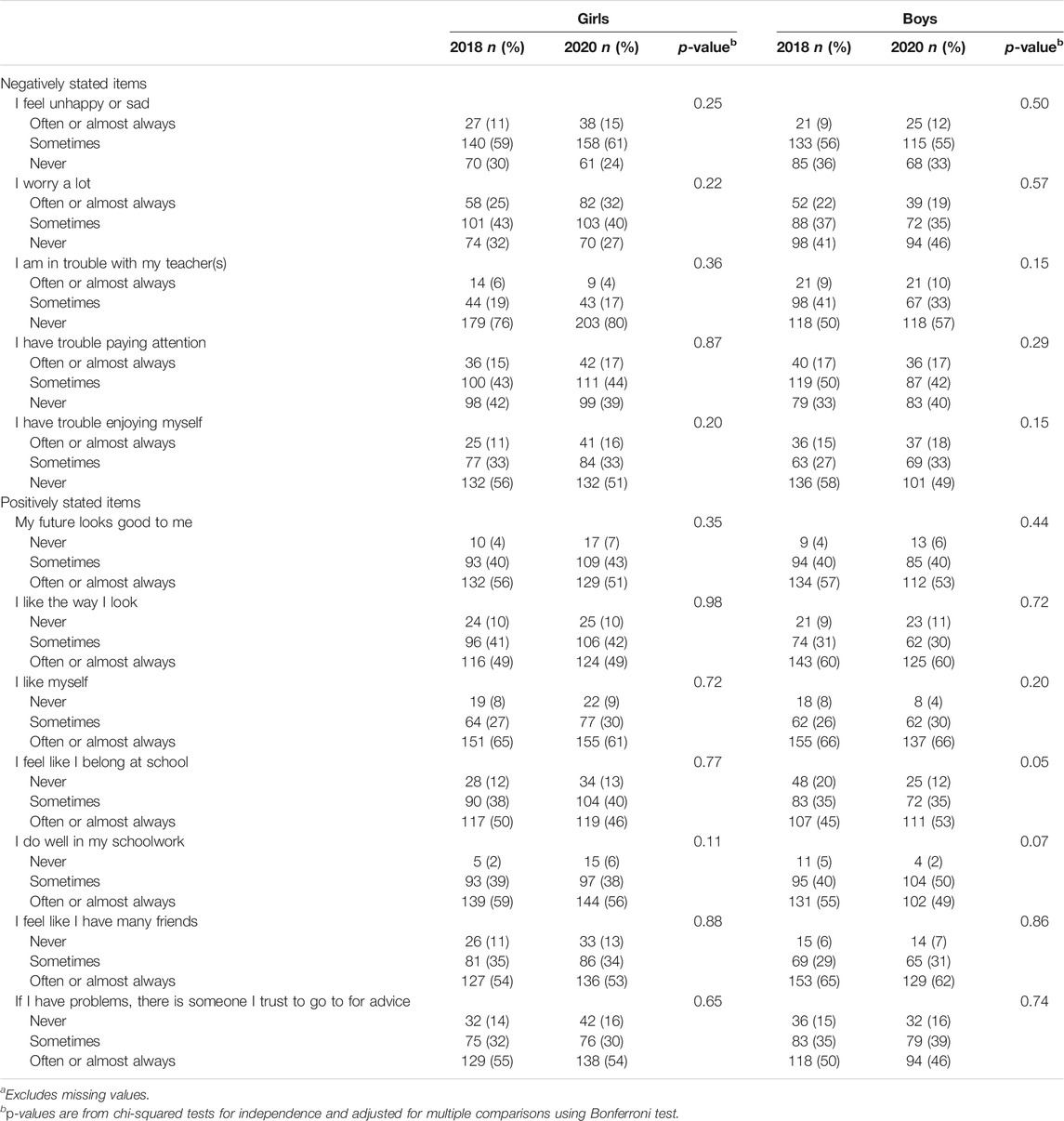
TABLE 2. Proportionsa of 9–12-year-old student responses to mental health and wellbeing items before the pandemic and after the first lockdown and school reopening, separately for girls and boys, Canada, 2018–2020.
Based on the MHW score, there was a modest decline in mental health and wellbeing among girls (4.9 [SD = 4.6] in 2018 vs. 4.4 [SD = 4.5] in 2020), however it did not attain statistical significance. There was no difference in the MHW score among boys: 4.8 (SD = 4.4) in 2018 vs. 4.8 (SD = 4.4) in 2020. The distribution of the scores (Figure 1) shows modest differences around the mean among girls and boys, with very little differences at the extremes of the distribution. After adjustment for potential confounders, the differences between 2018 and 2020 remained small and not statistically significant, for both girls (odds ratio [OR] 1.05, 95% confidence interval [CI] 0.82–1.33) (Table 3) and boys (OR 1.01, 95% CI 0.79–1.29) (Table 4).
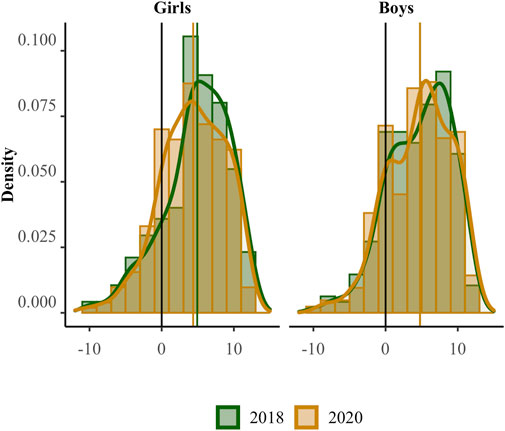
FIGURE 1. Distribution* of the cumulative mental health and well being score before the pandemic and after the first lockdown and school reopening, separately for girls and boys, Canada, 2018–2020. *Based on Kernel density estimator. Changes in mean scores: −0.57 (95% CI -1.38, 0.23) in girls; 0.01 (95% CI -0.81, 0.81) in boys.
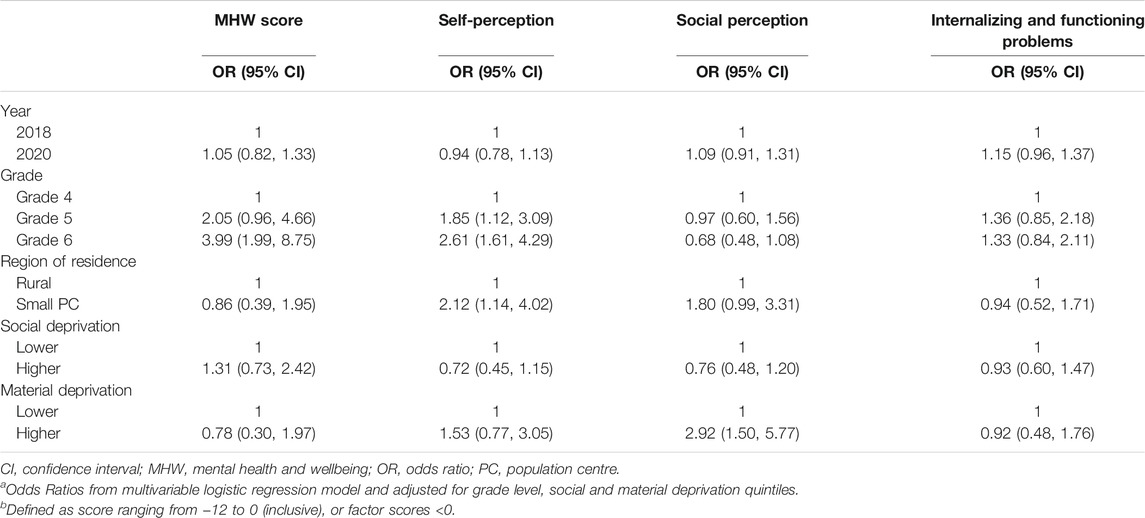
TABLE 3. Odds ratiosa (95% CI) of worse mental health and wellbeingb after the first lockdown and school reopening compared to before the pandemic among 9–12 year old girls, Canada, 2018–2020.
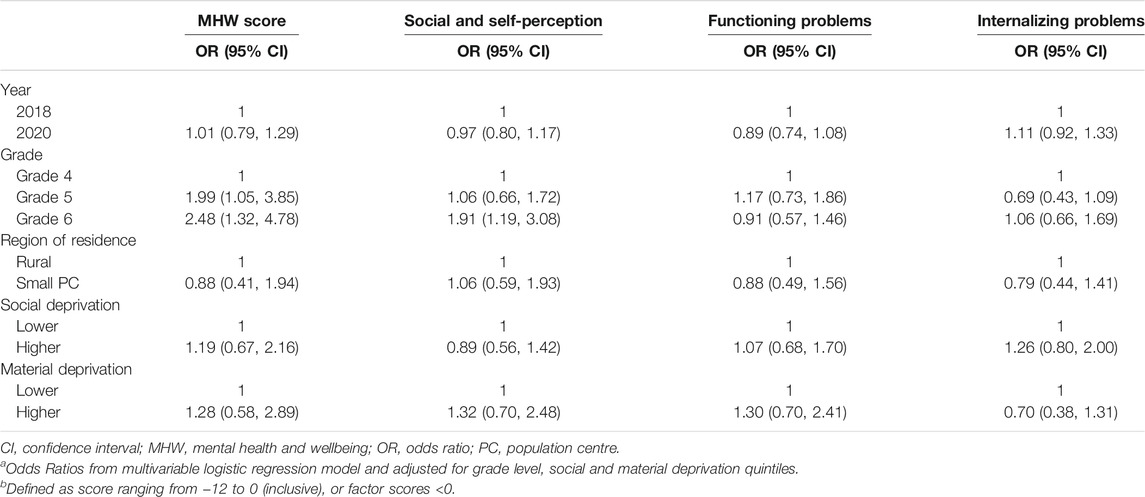
TABLE 4. Odds ratiosa (95% CI) of worse mental health and wellbeingb after the first lockdown and school reopening compared to before the pandemic among 9–12 year old boys, Canada, 2018–2020.
Three unique clusters of the 12 items were identified (Supplementary Table S1). The three factors among girls were labelled as self-perception, social perception, internalizing and functioning problems. The three factors among boys were labelled as social and self-perception, functioning problems, and internalizing problems. There were no statistically significant differences between 2018 and 2020 in any of the sub-groupings identified (Tables 3, 4). Finally, relative to those in grade 4, girls in grade 6 were more likely to report worse mental health and wellbeing and worse self-perception, whereas boys in grade 6 were more likely to report worse mental health and wellbeing and worse social and self-perception (Table 3 and 4).
Discussion
The present study revealed the lack of notable pre-pandemic vs. post-lockdown differences in mental health and wellbeing in a specific segment of children residing in rural and remote, socioeconomically disadvantaged communities. Evidence is emerging on the impact of the pandemic on mental health and wellbeing in the general populations of children and youth during the first lockdown. A recent study in a convenience sample of 168 school-aged children aged 7.6–11.6 years in the UK found a significant increase in depression symptoms, but not anxiety symptoms or emotional problems, during the first phase of the UK lockdown (April-June 2020), compared to the initial assessment 18 months prior to the lockdown [3]. In another study that collected responses to an online survey during a similar timeframe (May-June 2020) in Germany, 1,040 children and adolescents between 11 and 17 years old self-reported significantly more mental health problems (17.8 vs. 9.9%) and higher anxiety levels (24.1 vs. 14.9%) than in another representative sample of German adolescents (n = 1,556) assessed well before the pandemic, in 2017. Compared to their counterparts from higher socioeconomic backgrounds, children and youth from low socioeconomic backgrounds, recent migrants or refugees, and those with constrained living arrangements were at a significantly higher risk of experiencing anxiety and depressive symptoms during the lockdown [27].
Our findings of no substantial impact on children’s mental health and wellbeing post-lockdown are encouraging. We note that we surveyed students in November-December 2020—two to 3 months after schools were reopened. This window may have provided students enough time to adjust to the public health measures put in place to limit in-school transmission, while stressors related to school closure, being at home and separated from peers ceased. In addition, all schools were part of the APPLE Schools program that continued their health promotion activities to empower students in maintaining good health throughout the pandemic. While healthy eating activities such as taste testing and cooking classes were particularly challenging to deliver due to the COVID-19 safety protocols, a greater emphasis was placed on activities promoting mental health and wellbeing during this time [28, 29]. The APPLE Schools program had shared resources promoting mental health and wellbeing on schools’ social media pages, offering online activities (e.g., guided meditations, virtual days focusing on positive messages), art-based assignments (e.g., window art, virtual music days and talent shows), support from mental health therapists, among others. Moreover, resilience at the community level may also have helped to mitigate the negative impact of the public health measures. In addition to common strategies (e.g., positive peer and family interactions, positive self-identity), children and youth living in rural and remote areas rely on community-based resilience that is grounded in community connectedness [30]. This fundamental feature of rural and remote communities has become prominent during the pandemic: in some cases, these communities were much more proactive in COVID-19 response compared to urban areas [31].
Strengths of this study are that we surveyed a specific segment of children residing in socioeconomically disadvantaged areas, and achieved high responses rates. Although the 12 items and their cumulative score demonstrated high internal consistency in previous studies [32], they were not designed to capture pandemic-specific stressors and the public health measures put in place. Instead, these items are suitable to administer in the general (rather than clinical) populations of school-aged children in school-based research, and serve as a precursor to early onset of mental health outcomes (depression, anxiety, conduct disorder, and attention-deficit/hyperactivity disorder) [33]. While we employed a repeated cross-sectional study design, which is the design of choice when estimating trends over time, future research based on cohort studies of vulnerable children and youth will help reveal potential long-term negative psychosocial outcomes that might emerge from the stressors surrounding the pandemic, the limited social interactions and disrupted education [34]. Additionally, without a comparison or control schools, it is not possible to attribute the APPLE Schools health promotion programming to mental health and wellbeing outcomes. Lastly, we did not take into account seasonal effects that might have enhanced the comparability of two waves included in this study.
In sum, as children returned to school in Fall 2020 after the first COVID-19 lockdown was lifted, their mental health and wellbeing appear to return to pre-pandemic levels, similar to the levels observed among their peers pre-pandemic. The findings suggest that support for schools to tailor existing school-based health promotion programs and introduce new initiatives that encourage regular daily routine, healthy and active lifestyles, stimulate peer interaction and promote mental wellness in the school environment may help mitigate the effects of the pandemic on children’s mental health and wellbeing. It is critical to ensure schools are equipped with adequate capacity (e.g., staff training, resources, funding) to deliver enhanced school programming and supports for student mental health and wellbeing throughout the pandemic. Similarly, supporting communities, particularly those located in disadvantaged areas, to reduce economic stressors [35] and to foster resilience may help minimize the impact of future pandemics or other disasters on children’s mental health and wellbeing. These findings also align with recent calls that emphasize the importance of in-school learning for children’s mental health and wellbeing, especially for older and disadvantaged children. While recognizing that school closures may be an important factor in controlling the COVID-19 outbreaks, the international organizations and professional pediatric societies urge that schools should remain open as long as possible during the pandemic response [36–40].
Ethics Statement
The studies involving human participants were reviewed and approved by The Health Research Ethics Board of the University of Alberta (Pro00061528). Written informed consent for participation was not provided by the participants’ legal guardians/next of kin because: All students provided assent and their parents/guardians provided active-information passive-permission consent. The Health Research Ethics Board of the University of Alberta (Pro00061528) and participating school boards approved all the procedures.
Author Contributions
All listed authors contributed to study design, drafted and revised the article, and gave their final approval of the version submitted for publication. KM and PV conceptualized the study and methodology, and secured funding and resources. MK, KM, and PV developed a statistical analysis plan, and MK conducted all data analyses. JD and PV accessed and verified the data and wrote the original draft. All authors reviewed and approved the final manuscript.
Funding
The Public Health Agency of Canada (grant #1516-HQ-000071) along with other partners (for details see (41)) funded the APPLE Schools programming and data collection in the Northern communities. The present study was supported by operating funds from the Canadian Institutes for Health Research to KM and PV (grant #172685). KM holds the Murphy Family Foundation Chair in Early Life Interventions.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank the students, parents/guardians, and school principals for their participation in the research. They further thank teachers, school health facilitators and champions, project assistants, the APPLE School staff for facilitating the research, and specifically Tina Skakun, Katherine Dekker and Landra Walker for their major roles in coordinating and conducting the data collection.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2021.1604219/full#supplementary-material
References
1.United Nations. Policy Brief: Education during COVID-19 and beyond. [Internet] (2020). Available from: https://www.un.org/development/desa/dspd/wp-content/uploads/sites/22/2020/08/sg_policy_brief_covid-19_and_education_august_2020.pdf (cited 2021 Feb 9).
2.European Centre for Disease Prevention and Control. COVID-19 in Children and the Role of School Settings in COVID-19 Transmission. [Internet]. Stockholm, Sweden: European Centre for Disease Prevention and Control (2020). Available from: https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-schools-transmission-August%202020.pdf (Accessed August 23, 2021).
3. Bignardi, G, Dalmaijer, ES, Anwyl-Irvine, AL, Smith, TA, Siugzdaite, R, Uh, S, et al. Longitudinal Increases in Childhood Depression Symptoms during the COVID-19 Lockdown. Arch Dis Child (2020) 0:1–7. doi:10.1136/archdischild-2020-320372
4. Smetanin, P, Stiff, D, Briante, C, Adair, CE, Ahmad, S, and Khan, M. The Life and Economic Impact of Major Mental Illnesses in Canada. [Internet]. Toronto, ON: RiskAnalytica, on behalf of the Mental Health Commission of Canada (2011). Available from: https://www.mentalhealthcommission.ca/sites/default/files/MHCC_Report_Base_Case_FINAL_ENG_0_0.pdf (cited 2019 May 25).
5.SickKids. COVID-19: Guidance for School Operation during the Pandemic. [Internet] (2021). Available from: https://www.sickkids.ca/en/news/archive/2021/covid19-updated-guidance-school-operation-during-pandemic/ (cited 2021 Feb 23).
6. Cost, KT, Crosbie, J, Anagnostou, E, Birken, CS, Charach, A, Monga, S, et al. Mostly Worse, Occasionally Better: Impact of COVID-19 Pandemic on the Mental Health of Canadian Children and Adolescents. Eur Child Adolesc Psychiatry (2021) 1. doi:10.1007/s00787-021-01744-3
7. Vizard, T, Sadler, K, Ford, T, Newlove-Delgado, T, McManus, S, Marcheselli, F, et al. Mental Health of Children and Young People in England. [Internet] (2020). Available from: https://files.digital.nhs.uk/CB/C41981/mhcyp_2020_rep.pdf (cited 2021 Jun 28).
8.Statistics Canada. Labour Market Impacts of COVID-19 on Indigenous People. [Internet] (2020). Available from: https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00085-eng.htm (cited 2021 Feb 13).
9. Gassman-Pines, A, Ananat, EO, and Fitz-Henley, J. COVID-19 and Parent-Child Psychological Well-Being. Pediatrics (2020) 146(4):e2020007294. doi:10.1542/peds.2020-007294
10. Thakur, A. Mental Health in High School Students at the Time of COVID-19: A Student's Perspective. J Am Acad Child Adolesc Psychiatry (2020) 59(12):1309–10. doi:10.1016/j.jaac.2020.08.005
11. Loades, ME, Chatburn, E, Higson-Sweeney, N, Reynolds, S, Shafran, R, Brigden, A, et al. Rapid Systematic Review: the Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatry (2020) 59(11):1218–39. doi:10.1016/j.jaac.2020.05.009
12. Fung, C, Kuhle, S, Lu, C, Purcell, M, Schwartz, M, Storey, K, et al. From "best Practice" to "next Practice": the Effectiveness of School-Based Health Promotion in Improving Healthy Eating and Physical Activity and Preventing Childhood Obesity. Int J Behav Nutr Phys Act (2012) 9(1):27. doi:10.1186/1479-5868-9-27
13.Pan-Canadian Joint Consortium for School Health. Comprehensive School Health Framework. [Internet] (2016). Available from: http://www.jcsh-cces.ca/images/What_is_Comprehensive_School_Health_-_2-pager_-_July_2016.pdf (cited 2020 Jun 4).
14. Vander Ploeg, KA, Wu, B, McGavock, J, and Veugelers, PJ. Physical Activity Among Canadian Children on School Days and Nonschool Days. J Phys Act Health (2012) 9(8):1138–45. doi:10.1123/jpah.9.8.1138
15. Ekwaru, JP, Ohinmaa, A, Dabravolskaj, J, Maximova, K, and Veugelers, PJ. Cost-Effectiveness and Return on Investment of School-Based Health Promotion Programmes for Chronic Disease Prevention. Eur J Public Health (2021) 6:ckab130. doi:10.1093/eurpub/ckab130
16. Vander Ploeg, KA, Maximova, K, McGavock, J, Davis, W, and Veugelers, P. Do school-based Physical Activity Interventions Increase or Reduce Inequalities in Health? Soc Sci Med (2014) 112:80–7. doi:10.1016/j.socscimed.2014.04.032
17. Vander Ploeg, KA, McGavock, J, Maximova, K, and Veugelers, PJ. School-based Health Promotion and Physical Activity during and after School Hours. Pediatrics (2014) 133(2):e371–e378. doi:10.1542/peds.2013-2383
18. Ofosu, NN, Ekwaru, JP, Bastian, KA, Loehr, SA, Storey, K, Spence, JC, et al. Long-term Effects of Comprehensive School Health on Health-Related Knowledge, Attitudes, Self-Efficacy, Health Behaviours and Weight Status of Adolescents. BMC Public Health (2018) 18(1):515. doi:10.1186/s12889-018-5427-4
20. Marsh, HW, and O'Neill, R. Self Description Questionnaire III: the Construct Validity of Multidimensional Self-Concept Ratings by Late Adolescents. J Educ Meas (1984) 21(2):153–74. doi:10.1111/j.1745-3984.1984.tb00227.x
21. Rosenberg, M. Society and the Adolescent Self-Image. Princeton, NJ: Princeton University Press (1965).
22.Statistics Canada. National Longitudinal Survey of Children and Youth (NLSCY). Catalogue No. 89F0077XIE. Statistics Canada (1995) (Report No.: 89F0077XIE). Available from: http://www23.statcan.gc.ca/imdb-bmdi/instrument/4450_Q1_V1-eng.pdf (Accessed August 23, 2021).
23.Statistics Canada. Population centre (POPCTR): Detailed Definition. [Internet] (2018). Available from: https://www150.statcan.gc.ca/n1/pub/92-195-x/2011001/geo/pop/def-eng.htm (cited 2021 Feb 8).
24. Pampalon, R, and Raymond, G. A Deprivation index for Health and Welfare Planning in Quebec. Chronic Dis Can (2000) 21(3):104–13.
25. van Buuren, S, and Groothuis-Oudshoorn, K. MICE: Multivariate Imputation by Chained Equations in R. J Stat Softw (2011) 45(3):1–67. doi:10.18637/jss.v045.i03
26. Clark, TS, and Linzer, DA. Should I Use Fixed or Random Effects? Psrm (2015) 3(2):399–408. doi:10.1017/psrm.2014.32
27. Ravens-Sieberer, U, Kaman, A, Erhart, M, Devine, J, Schlack, R, and Otto, C. Impact of the COVID-19 Pandemic on Quality of Life and Mental Health in Children and Adolescents in Germany. Eur Child Adolesc Psychiatry (2021) 1. doi:10.1007/s00787-021-01726-5
28. Loewen, OK, Maximova, K, Ekwaru, JP, Faught, EL, Asbridge, M, Ohinmaa, A, et al. Lifestyle Behavior and Mental Health in Early Adolescence. Pediatrics (2019) 143(5):e20183307. doi:10.1542/peds.2018-3307
29. Wu, X, Bastian, K, Ohinmaa, A, and Veugelers, P. Influence of Physical Activity, Sedentary Behavior, and Diet Quality in Childhood on the Incidence of Internalizing and Externalizing Disorders during Adolescence: a Population-Based Cohort Study. Ann Epidemiol (2018) 28(2):86–94. doi:10.1016/j.annepidem.2017.12.002
30. Toombs, E, Kowatch, KR, and Mushquash, CJ. Resilience in Canadian Indigenous Youth: a Scoping Review. Int J Child Adolesc Resil (2016) 4(1):4–32.
31. Power, T, Wilson, D, Best, O, Brockie, T, Bourque Bearskin, L, Millender, E, et al. COVID-19 and Indigenous Peoples: an Imperative for Action. J Clin Nurs (2020) 29(15–16):2737–41. doi:10.1111/jocn.15320
32. Maximova, K, Khan, MKA, Austin, SB, Kirk, SFL, and Veugelers, PJ. The Role of Underestimating Body Size for Self-Esteem and Self-Efficacy Among Grade Five Children in Canada. Ann Epidemiol (2015) 25(10):753–9. doi:10.1016/j.annepidem.2015.07.009
33. Thomson, KC, Richardson, CG, Gadermann, AM, Emerson, SD, Shoveller, J, and Guhn, M. Association of Childhood Social-Emotional Functioning Profiles at School Entry with Early-Onset Mental Health Conditions. JAMA Netw Open (2019) 2(1):e186694. doi:10.1001/jamanetworkopen.2018.6694
34. Jones, B, Woolfenden, S, Pengilly, S, Breen, C, Cohn, R, Biviano, L, et al. COVID ‐19 Pandemic: The Impact on Vulnerable Children and Young People in Australia. J Paediatr Child Health (2020) 56(12):1851–5. doi:10.1111/jpc.15169
35. Zajacova, A, Jehn, A, Stackhouse, M, Choi, KH, Denice, P, Haan, M, et al. Mental Health and Economic Concerns from March to May during the COVID-19 Pandemic in Canada: Insights from an Analysis of Repeated Cross-Sectional Surveys. SSM - Popul Health (2020) 12:100704. doi:10.1016/j.ssmph.2020.100704
36. Fore, HH. Children Cannot Afford Another Year of School Disruption. [Internet]. UNICEF (2021). Available from: https://www.unicef.org/press-releases/children-cannot-afford-another-year-school-disruption (cited 2021 Apr 26).
37.World Health Organization. Considerations for School-Related Public Health Measures in the Context of COVID-19. [Internet] (2020). Available from: https://www.who.int/publications-detail-redirect/considerations-for-school-related-public-health-measures-in-the-context-of-covid-19 (cited 2021 Feb 23).
38.UNESCO. UNESCO Figures Show Two Thirds of an Academic Year Lost on Average Worldwide Due to Covid-19 School Closures. [Internet] (2021). Available from: https://en.unesco.org/news/unesco-figures-show-two-thirds-academic-year-lost-average-worldwide-due-covid-19-school (cited 2021 Apr 26).
39.American Academy of Pediatrics. COVID-19 Guidance for Safe Schools. [Internet] (2021). Available from: http://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-planning-considerations-return-to-in-person-education-in-schools/ (cited 2021 Feb 23).
40.European Academy of Pediatrics. COVID-19 and Children: A Call from Paediatric Leaders across Europe. [Internet]. Available from: https://www.eapaediatrics.eu/wp-content/uploads/2020/07/DFTB-4990-EAPS-leaflet-02b.pdf (Accessed August 23, 2021).
41.APPLE Schools. APPLE Schools Is an Innovative School-Focused Health Promotion Initiative. [Internet] (2021). Available from: https://www.appleschools.ca/ (cited 2021 Feb 3).
Keywords: health promotion, public health, children, social determinansts of health, COVID–19, internalizing problems, school health, mental health and wellbeing
Citation: Dabravolskaj J, Khan MKA, Veugelers PJ and Maximova K (2021) Mental Health and Wellbeing of 9–12-year-old Children in Northern Canada Before the COVID-19 Pandemic and After the First Lockdown. Int J Public Health 66:1604219. doi: 10.3389/ijph.2021.1604219
Received: 27 April 2021; Accepted: 17 August 2021;
Published: 01 September 2021.
Edited by:
Franco Mascayano, Columbia University Irving Medical Center, United StatesReviewed by:
Anthony Jehn, Western University, CanadaSally McManus, City University of London, United Kingdom
Copyright © 2021 Dabravolskaj, Khan, Veugelers and Maximova. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paul J. Veugelers, cGF1bC52ZXVnZWxlcnNAdWFsYmVydGEuY2E=
†ORCID: Julia Dabravolskaj, orcid.org/0000-0002-4420-668X; Mohammed KA Khan, orcid.org/0000-0003-2354-971X; Paul J. Veugelers, orcid.org/0000-0001-8996-0822; Katerina Maximova, orcid.org/0000-0001-9842-1927
 Julia Dabravolskaj1†
Julia Dabravolskaj1†