Abstract
Objectives: This study aims to provide a systematic review and meta-analysis of the literature on the long-term effects of interventions addressing children’s and adolescents’ mental health literacy and/or stigmatizing attitudes.
Methods: Articles in English or German published between January 1997 and May 2020 were retrieved from five databases, leading to a total of 4,375 original articles identified.
Results: 25 studies were included after applying exclusion criteria, 13 of which were eligible for meta-analysis. The overall average of the follow-up period was about 5 months. Long-term improvements were sustained for mental health literacy, d = 0.48, 95% CI = (0.34, 0.62), as well as for stigmatizing attitudes, d = 0.30, 95% CI = (0.24, 0.36), and social distance, d = 0.16, 95% CI = (0.03, 0.29). The combination of educational and contact components within interventions led to worse results for mental health literacy, but not stigmatizing attitudes or social distance.
Conclusion: Interventions targeting children and adolescents generally have a brief follow-up period of an average of 5 months. They show a stable improvement in mental health literacy, but are to a lesser degree able to destigmatize mental illness or improve social distance.
Introduction
Most mental disorders emerge during childhood and adolescence. An estimated 75% of mental disorders have an onset before the age of 25, with 50% developing before the age of 14 [1]. Beyond the distress and impairment of mental disorders, they also have disruptive effects on academic achievement, personal relationships, and stability within the job market, bringing about negative social and financial consequences lasting into adulthood. Negative consequences do not only affect individuals during their experience of mental disorder, but can influence their mental health trajectory later in life [2, 3].
Globally, there exists a discrepancy between the need for mental health services and their (low) availability and utilization at all ages, with different impeding factors, e.g., limited resources or mental health knowledge [4]. In this paper, we focus particularly on two constructs considered as key factors for improving this situation: mental health literacy (MHL) and stigma.
MHL was first defined by Jorm et al. [5] as the “knowledge and beliefs about mental disorders which aid their recognition, management or prevention.” As such, it has been identified as a significant predictor for seeking help via mental health services [6]. More specifically, Tully et al. [7] suggest that an important factor contributing to inadequate utilization of mental health treatment options, particularly among younger people, may be low MHL levels among parents and community members. However, MHL is both a social and individual resource that can be fostered in young people. From a public health perspective, empowering children and adolescents to seek help for mental problems is crucial for secondary and tertiary prevention of mental illness (i.e., as cure or disorder management).
The stigma associated with mental illness also presents a significant barrier to help-seeking processes and has been described as “having worse consequences than the conditions themselves” [8]. This is partly because widespread prejudice and stereotypes (e.g., that those with mental illness are weak, dangerous, or inept) bring about discrimination on institutional and individual levels—for example, in the workplace, the health care system, or everyday social interactions [9]. Exposed to such stereotypes, people affected by mental illness may also stigmatize themselves, leading to low self-esteem, low self-efficacy, negative emotional reactions, and corresponding behaviors that further reduce quality of life [10]. In turn, self-stigma and/or fear of stigma can influence individuals to avoid seeking help in treatment form, with consequences for their further mental health [11].
As outlined, the prevalence of help-seeking behaviors when experiencing signs of mental illness is assumed to be deeply connected to perceived public perceptions of mental illness, including stigmatizing attitudes. Accordingly, stigma has frequently been examined in mental illness studies [12]. While many interventions for the improvement of mental health among children and adolescents exist, O’Reilly et al. [13] have called the lacking evidence base and the question of their long-term efficacy to attention. Moreover, while interventions tackling stigma have been reviewed more often [14–16], less knowledge is available for MHL. At the same time, to our knowledge, the existing reviews on interventions for MHL improvement in children and adolescents, do not tackle the question of long-term effectiveness. Important contributions in the MHL field, differing in aim and scope, were conducted by Wei et al. [17] (assessing general intervention effectiveness), Seekadet et al. [18] (assessing intervention types’ effectiveness), and Patafio et al. [19] (providing an overview of intervention programs). Some limitations of the Wei et al. [17] and Patafio et al. [19] studies were their inclusion of studies lacking control conditions, indicating weaker study designs and less accurate results. In contrast, this review only includes studies with control conditions and focuses specifically on long-term intervention effectiveness.
Aim
We aim to provide a systematic review and meta-analysis of interventions that aim to improve young peoples’ MHL and/or to reduce mental illness related stigma in the target group. We investigate MHL and stigma as separate but possibly related outcomes of intervention programs, while acknowledging that—as currently understood—MHL is a multidimensional construct that may incorporate stigma among other aspects. However, we regard MHL and stigma as distinct outcomes to avoid the ambiguity and heterogeneity that arises when studies measuring distinct aspects are summarized under the overarching label “MHL” [20].
Additionally, to narrow the knowledge gap regarding long-term effects of intervention studies [14, 15], our focus lies on interventions that follow up on their results by incorporating three measurement time points.
Research question: Do mental health intervention programs addressing children and adolescents effectively 1) reduce stigma related to mental illness and/or 2) improve MHL long-term?
Methods
Search Methodology
To find evaluated interventions addressing mental health-related stigma and/or MHL in children and adolescents, the following databases were searched for articles in English or German published from 1997 onward—when the term “mental health literacy” was introduced by Jorm et al. [5]: PubMed, PsycINFO, PSYNDEX, ERIC, and Web of Science Core Collection. PubMed and Web of Science were searched directly; the others were accessed via the research platform EBSCOhost. One search phase was conducted by searching for articles published between 1997 and May 2018 by two of our researchers. Since we were unable to finalize the publication due to time constraints, we added another search phase between May 2018 and May 2020 to keep results current. During both search phases, the same search algorithm was used.
The search strategy was developed through an iterative process with team members. Feedback was also obtained from librarians and external experts. The search term was adapted for each database. See Supplementary Figure S1 of the supplementary material for an example of the search string used in PubMed.
Additionally, a manual search was conducted by contacting experts and organizations and manually searching through the references of key publications found through the database search.
Inclusion and Exclusion Criteria
Studies were included if they:
1) addressed children and adolescents. Although we chose the legal age of consent of 18 years as an orientation point, we did not exclude studies with a few participants older than 18,
2) included three measurement points: one pre-intervention point, one post-intervention point and one follow-up assessment,
3) delivered an intervention program,
4) had a control group or provided an intervention as treatment as usual,
5) assessed the mental health-related stigma and/or MHL directly through the self-report of children or adolescents, instead of relying on information from caregivers or teachers.
Studies were excluded if they:
1) had no information about participants’ age or affiliation to the educational system (so it could not be inferred whether they were underaged),
2) did not directly measure the MHL and/or stigma for children and adolescents, but through representatives such as parents or teachers,
3) did not report results (e.g., abstracts of registered clinical trials).
Selection Process
The identified citations, together with their bibliographic records, such as title, abstract, and keywords, were imported from the databases into a reference management program.
First, duplicate publications were automatically removed by the program and manually verified in two phases by two researchers. Second, 200 abstracts were jointly screened by the same researchers to establish the rate of agreement between them. The initial interrater reliability resulted in an overlap of 86.5% and after disagreements were discussed, it was optimized to 100% in a second joint screening.
Third, title/abstract screening was performed independently by the same two researchers in the first phase and independently by one of them in the second phase. One researcher screened the PsycINFO and Web of Science results, while another screened those from PubMed, ERIC, and PSYNDEX. In the second phase, all databases were searched by one researcher.
Fourth, the full texts of the included studies were obtained through the university library. If articles were inaccessible, their authors were contacted. Full-text screening was then conducted by the same two researchers together in the first phase and by one of them in the second phase. Uncertainties regarding study eligibility were resolved through discussion between the two researchers until a consensus on inclusion or exclusion was reached. Finally, information from the included articles was extracted into tables created for this review. These tables cover characteristics of the sample and characteristics of the intervention.
Quality Assessment
Two authors rated the included studies’ quality using the Checklist for quality assessment of controlled intervention studies, a free resource from the National Heart, Blood and Lung Institute [21] comprising 14 questions. They rated each question and resolved discrepancy through discussion. The overall assessment was based on a point system factoring in the checklist’s guiding elements. One question regarding participant blinding was not included in calculation of the final score, as in most cases, blinding is not feasible when providing educational interventions. Moreover, we complemented the intervention fidelity assessment criteria with the criterion of a training provision for the facilitators of an intervention. This, however, was also omitted from the final score. One point was given for each question answered with “yes” except for question 13 regarding the prior specification of reported outcomes or subgroups. Here, we differentiated more distinctly between two possibilities. Studies with a preregistered study protocol were granted one point; studies mentioning the change of predefined outcomes as a study aim were granted 0.5 points. The possible final score could range from zero points, indicating a very high risk of bias, to 13 points, indicating a low risk of bias.
Data Analysis
We computed weighted means for the follow-up lengths and participants’ ages. When the follow-up period was reported as a range, we used the mean of that range. We intended to calculate odds ratios for dichotomous outcomes, but this applied to only two studies. We verified which studies reported means and standard deviations for the main outcomes and included those into a meta-analysis using a random effects model. The analysis was conducted by one author using STATA 16 [22]. Due to the heterogeneity of measurement tools, the measured outcomes were regrouped into three categories [1]: MHL [2], stigmatizing attitudes, and [3] social distance. Higgins’s I2 test was used to estimate “the proportion of variation between the sample estimates that is due to heterogeneity rather than to sampling error” [23]. If I2 has a value of 50% or more it is considered to have significant heterogeneity [23].
The categories were built through inductive reasoning, considering both conceptualization and operationalization of the measures used. When articles did not explicitly mention the construct measured, the measurement instruments were carefully considered and categorized as follows:
• MHL: items regarding knowledge,
• stigma: items about attitudes (e.g., agreement regarding stereotypes about mental illness), and
• social distance: willingness to interact with a person with mental illness in varying contexts.
More detailed differentiation in terms of MHL (e.g., separating general MHL and more specific knowledge on particular disorders, e.g., depression literacy, etc.) and stigma (e.g., self-stigma) was considered, however, too few studies were available to support this categorization.
Moreover, we verified whether the length of post- or follow-up assessment affected the outcomes with linear meta-regression. We also assessed a possible effect of the intervention type (educational intervention vs. educational plus contact intervention) and study design [randomized controlled-trials (RCT) vs. non-RCT].
Results
The search provided 6,345 records, of which 1,975 were duplicates. The manual search revealed an additional 5 articles. The screening and selection process is illustrated in more detail in Figure 1. In total, 25 studies were included for the analysis. Ten studies measured stigma only, three studies MHL only, while twelve studies assessed both.
FIGURE 1
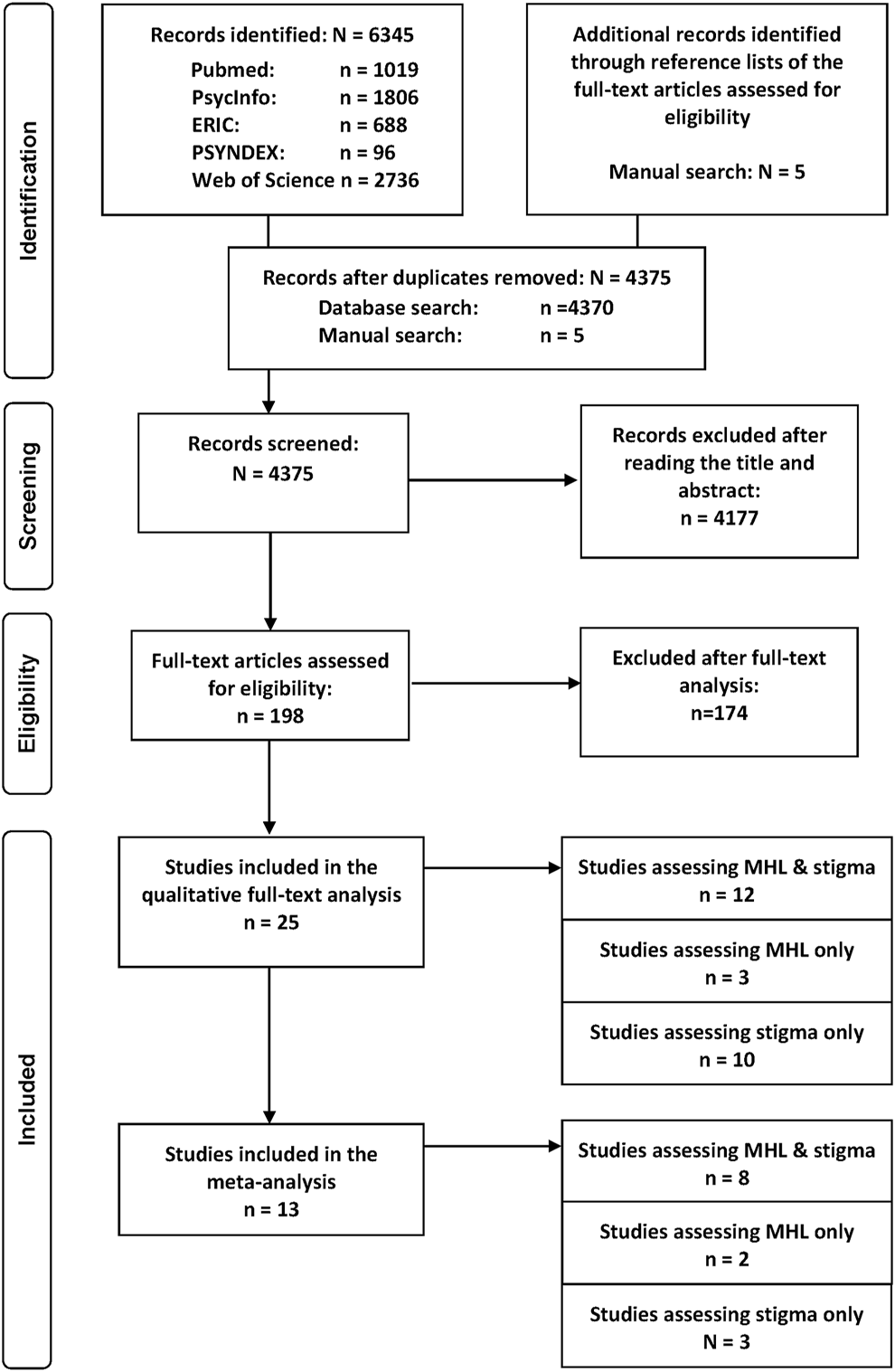
Prisma flow-chart of papers included in the review regarding the long-term effectiveness of interventions addressing mental health literacy and stigma of mental illness in children and adolescents, search period: January 1997 to May 2020. Project: Improving mental health literacy to reduce stigma (IMPRES), Bielefeld, Germany, 03.2018 - 02.2021.
17 studies were retrieved during the first search period (up until May 2018) and 8 during the second search period (from May 2018 to May 2020). As defined in the inclusion/exclusion criteria, all of the studies employed three measurement time points. However, this only applied to the intervention group. Four studies used only two measurement points in the control group [numbers (nos.) 1, 5, and 11 did not have a follow-up measurement, while no. 6 did not measure the post-assessment, but directly the follow-up], but were not excluded in order to maintain a larger database. On average, the follow-up time was 5 months after intervention finalization. When studies reported more than two post-measurement time points, the first and the last post-test measurements were considered.
Descriptive Summary of Included studies
A summary of key study characteristics is displayed in Table 1 and descriptions of each study can be found in Table 2.
TABLE 1
| All studies included in the review (n = 25) | Only studies eligible for meta-analysis (n = 13) | |
|---|---|---|
| Sample size | n = 18,157 | n = 6528 |
| Study design | 52% used a randomized controlled design (at different levels: school, class, participant) | 38.5% used a randomized controlled design (at different levels: school, class, participant) |
| Length of follow-up in weeks | m = 23.14 (weighted) | m = 23.73 (weighted) |
| range = 4.3 to 103.2 | range = 6 to 103.2 | |
| Participants’ age | m = 14.55 (weighted), range = 9–21 | m = 14.50 (weighted), range = 9–18 |
| Continent | • Europe: 9 studies | • Australia: 5 studies |
| • North America: 6 studies | • North America: 4 studies | |
| • Australia: 7 studies | • Europe: 2 studies | |
| • Asia: 3 studies | • Asia: 2 studies | |
| Setting | 76% of studies were conducted in school, while others were conducted in the community, in school/sport clubs, or with clinical population | 69.23% of studies were conducted in school, while others were conducted in the community, in school/sport clubs, or with clinical population |
| Type of administered intervention | • educational intervention: 11 studies | • educational intervention: 8 studies |
| • educational and contact intervention: 10 studies (in person contact: 8 studies, in person + video contact: 1 study, video contact: 1 studies) | • educational and contact intervention: 3 studies (personal contact: 2 studies, in person + video contact: 1 study) | |
| • comparison between education and education + contact intervention: 1 study | • indirect intervention trough parental training: 1 study | |
| • contact intervention (video): 1 study | • unknown: 1 study | |
| • indirect intervention through parental training: 1 study | ||
| • unknown: 1 study | ||
| General intervention topic | • general MH: 17 studies | • general MH: 9 studies |
| • specific MH: 7 (depression 4, schizophrenia 3) | • specific MH: 3 (depression 3) | |
| • unknown: 1 study | • unknown: 1 study | |
| Duration of intervention | range: <1–18 h | range: <1–18 h |
| • up to 1 h: 5 studies | • up to 1 h: 1 study | |
| • > 1–5 h: 8 studies | • > 1–5 h: 5 studies | |
| • > 5–9 h: 3 studies | • > 5–9 h: 0 studies | |
| • > 9 h: 6 studies | • > 9 h: 4 studies | |
| • unknown: 3 studies | • unknown: 3 studies | |
| Timespan of intervention | range: 1 day to 2,5 months | range: 1 day to 2,5 months |
| • up to 1 day: 10 studies | • up to 1 day: 3 studies | |
| • > 1 day, < 1 week: 6 studies | • > 1 day, < 1 week: 5 studies | |
| • > a week, < a month: 2 studies | • > a week, < a month: 0 studies | |
| • > a month: 4 studies | • > a month: 3 studies | |
| • unknown: 3 studies | • unknown: 2 studies | |
| Person who delivered intervention | • (MH) professional [5]/teacher [1]/researcher [1]/unknown [1] + person with personal experience: 8 studies | • (MH) professional [1]/teacher [1] + person with personal experience: 2 studies |
| • teacher (+researcher [1]): 5 studies | • teacher (+researcher [1]): 4 studies | |
| • (MH) professional: 4 studies | • (MH) professional: 3 studies | |
| • trained presenter: 3 Studies | • trained presenter: 1 Studies | |
| • person with personal experience: 2 studies | • person with personal experience: 1 study | |
| • unknown: 4 studies (note: n = 26; one study used two different delivery persons to compare modes) | • unknown: 3 studies (note: n = 14; one study used two different delivery persons to compare modes) | |
| Didactic materials | Multi-method: 21 studies; primarily one method: 2 studies; unknown: 2 studies | Multi-method: 10 studies; primarily one method: 1 study; unknown: 2 studies |
| • informative/educational presentations: 21 | • informative/educational presentations: 11 | |
| • exercises/games/role-plays: 15 studies | • exercises/games/role-plays: 8 studies | |
| • guided discussions: 12 | • guided discussions: 5 | |
| • Q&A session regarding personal experience with MI: 9 studies | • Q&A session regarding personal experience with MI: 4 studies | |
| • informative video: 8 | • informative video: 4 |
Studies assessing the long-term effects on MHL and/or stigma in children or adolescents: a summary of intervention/study characteristics, search period: January 1997 to May 2020. Project: Improving mental health literacy to reduce stigma (IMPRES), Bielefeld, Germany, 03.2018 - 02.2021.
M, average; SD, standard deviation; MH, mental health; H, hour; Q&A, question and answer; MI, mental illness.
TABLE 2
| Study | Sample | Study design and outcomes | Intervention | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No.a | Authors | Country | Settingb | Participant age (mean) | Participant age (SD) | Participant age rangec | Sample sized | Length follow-up in weekse | Risk of biasf | Randomization | Assessed outcomesg | Outcome categorizationh | Type of interventioni | Intervention topicj |
| 1 | Ahmad et al. (2019) [20] | United States | school clubs | not reported | not reported | not reported | 545 | 15.05 | 3.5 | yes, at school level | MHL, S | MHL, SA, SD | unknown | unknown |
| 2 | Andrés-Rodríguez et al. (2017) [21] | Spain | school | 14.24 | 0.47 | 14–18 | 393 | 38.7 | 4.5 | no | S | SA, SD | E + C | general MH |
| 3 | Campos et al. (2018) [22] | Portugal | school | 13.04 | 0.79 | 12–14 | 543 | 25.8 | 2.5 | yes, at class level | MHL | MHL | E | general MH |
| 4 | Esters et al. (1998) [23] | United States | school | 14.7 | not reported | 13–17 | 40 | 12 | 2 | no | S | SA | E | general MH |
| 5 | Fraser et al. (2008) [24] | Australia | clinical population (parents and 1/3 children with MI) | 13.34 | 1.58 | 12–17 | 44 | 19 | 0.5 | no | MHL | MHL | E | general MH |
| 6 | Ibrahim et al. (2020) [25] | Malaysia | clinical population (symptoms of MI) | 14.61 | 1.39 | 13–17 | 101 | 12.9 | 4.5 | no | MHL, S | MHL, SA | E | specific MH: depression |
| 7 | Lai et al. (2016) [26] | China | school | 15.1 | 1 | 14–16 | 3391 | 19.35 | 4.5 | no | MHL, S | MHL SA | E | specific MH: depression |
| 8 | Morgan et al. (2019) [27] | Australia | community | 13.3 | 1.54 | 12–15 | 301 | 103.2 | 10 | yes, at participant level | S | SA, SD | indirect: E for parents | general MH |
| 9 | Perry et al. (2014) [28] | Australia | school | 14.8 | 0.73 | 13–16 | 380 | 25.8 | 7 | yes, at class level | MHL, S | MHL, SA | E | general MH |
| 10 | Pinto-Foltz et al. (2011) [29] | United States | school | 15 | 0.67 | 13–17 | 156 | 8 | 6.5 | yes, at class level | MHL, S | MHL, SD | E + C | general MH |
| 11 | Robinson et al. (2010) [30] | Australia | school | 15.2 | 0.5 | 14–16 | 246 | 10.6 | 1.5 | no | MHL, S | MHL, SA, SD | E + C (C in person and via video) | specific MH: depression |
| 12 | Ventieri et al. (2011) [31] | Australia | school | 10.67 | 0.89 | 9–12 | 195 | 17.2 | 1.5 | no | MHL, S | MHL, SA, SD | E | general MH |
| 13 | Wahl et al. (2011) [32] | United States | school | 12.5 | 0.6 | 7th, 8th grade | 193 | 6 | 1.5 | no | MHL, S | MHL, SA, SD | E | general MH |
| 14 | Campbell et al. (2010) [33] | United Kingdom | school | 14.64 | 0.48 | 14–15 | 92 | 10 | 6.5 | yes, at class level | S | SA | E + C | specific MH: psychosis (categorized as schizophrenia) |
| 15 | Chisholm et al. (2016) [34] | United Kingdom | school | 12.21 | 0.58 | 12–13 | 769 | 25.8 | 9 | yes, at class level | MHL, S | MHL, SD | E vs. E + C | general MH |
| 16 | Conrad et al. (2009) [35] | Germany | school | not reported | not reported | 13–18 | 210 | 12.9 | 1.5 | no | S | SD | E + C | general MH |
| 17 | Economou et al. (2011) [36] | Greece | school | 13.84 | 0.82 | 13–15 | 616 | 51.6 | 5.5 | yes, at class level | S | SA | E | specific MH: schizophrenia |
| 18 | Goncalves et al. (2015) [37] | Portugal | school | not reported | not reported | 7th, 8th, 9th grade | 207 | 4.3 | 3.5 | yes, at class level | S | SA, self-stigma | C (via video) | general MH |
| 19 | Hart et al. (2019) [38] | Australia | school | 15.87 | 0.52 | 15–17 | 1605 | 51.6 | 7 | yes, at school level | MHL | MHL | E | general MH |
| 20 | Liddle et al. (2021) [39] | Australia | football club | 14.3 | 1.75 | 12–18 | 102 | 4.3 | 9 | yes, at team/team-age level | MHL, S | MHL, SA | E + C | general MH |
| 21 | Mulfinger et al. (2018) [40] | Germany | clinical population (diagnosed with MI) | 15.75 | 1.63 | not reported | 98 | 6 | 9 | yes, at participant level within clusters | S | self-stigma | E + C | general MH |
| 22 | Ng et al. (2002) [41] | China | school | 15 | not reported | 13–21 | 169 | 30.1 | 3.5 | no | S | SA | E + C | general MH |
| 23 | Schulze et al. (2003) [42] | Germany | school | 15.1 | not reported | 14–18 | 150 | 4.3 | 1.5 | no | S | SA, SD | E + C | specific MH: schizophrenia |
| 24 | Swartz et al. (2017) [43] | United States | school | not reported | not reported | 14–15 | 6679 | 17.2 | 3 | yes, at school level | MHL, S | MHL, SD | E | specific MH: depression |
| 25 | Wahl et al. (2018) [44] | United States | school | 14.7 | not reported | 13–18 | 932 | 5 | 1.5 | no | MHL, S | MHL | E + C (C via video) | general MH |
Studies assessing the long-term effects on MHL and/or stigma in children or adolescents: a presentation of individual studies, search period: January 1997 to May 2020. Project: Improving mental health literacy to reduce stigma (IMPRES), Bielefeld, Germany, 03.2018 - 02.2021.
Studies no. 1 to 13 were included in the meta-analysis.
MI, mental illness.
where not available, school grade is reported.
at baseline of data collection.
where months were reported, the number was multiplied by 4.3; where only a timespan was mentioned, the average was used; if there were two follow-up timepoints the last one was reported.
Range: 0 to 13, higher scores indicating less risk of bias.
MHL, mental health literacy; S, stigma.
MHL, mental health literacy; SA, stigmatizing attitudes; SD, social distance.
E, education, C, contact.
MH, mental health.
The studies were conducted in nine different countries. All but six were conducted in schools, usually during regular lessons (other settings: clinical context: n = 3; football/school club: n = 2; community: n = 1). Most studies included both males and females, however two (nos. 11 and 20) targeted males only, while one targeted females only (no. 10). The average age was 14.55 years and ranged from nine to 21 years. A detailed description of the quality assessment of the included studies can be found in Supplementary Table S1 of the supplementary material. The average quality score was 4,4 (SD = 2,9).
Overall, two intervention types were predominant: educational interventions (n = 11) and educational plus contact interventions (n = 10). The remaining four studies had differing approaches: one compared educational and educational plus contact interventions (no. 15), one only contained contact with a person who experienced mental illness via video (no. 18), and one indirect intervention addressed parents (no. 8). Finally, in one study, the intervention type was not reported clearly (no. 1). Most interventions addressed general mental health topics (n = 17). Some targeted specific mental health issues, focusing on either depression (n = 4) or schizophrenia (n = 3).
Generally, interventions diverged in content and organization. Their durations ranged from under 1 h to a maximum of 18 h. Over half (13 out of 22) had a rather short duration of up to 5 h, while three studies did not report the intervention duration.
Considering the interventions’ timespans, most interventions (n = 10) can be described as short-term, i.e., delivered within 1 day. Eight were categorized as mid-term, lasting up to 1 week (n = 6) or up to 1 month (n = 2). The remaining four “long-term” interventions had a length of over 1 month.
A team of teachers and mental health professionals were frequently responsible for administering the interventions. One study compared effectiveness of delivery by mental health professionals to delivery by teachers (no. 7). Also, different modalities were used for delivering intervention content, including educational presentations and/or videos combined with various interactive parts (e.g., exercises, games, role-plays, guided discussions, etc). Some studies (n = 9) also included personal contact, where a person with mental illness experience shared their knowledge and responded to students’ questions.
Effectiveness of Interventions in Reducing Stigma and Improving MHL
Means and standard deviations were retrieved from studies where they were reported (n = 12). One author provided this data upon request (no. 13), however, we were unable to obtain additional information from the other studies. One study (no. 15) reported all necessary means, but did not have a control group, rather comparing two different versions of the same intervention. This study was excluded from meta-analysis since it would have skewed effectiveness.
One of the studies (no. 7) compared two different delivery options of the same intervention (i.e., implemented by professionals vs. by teachers) and included a control group. We divided this study into two separate entries, using the same control group as a reference. Therefore, when reporting the number of participants on which each outcome was based, we subsequently subtracted the equivalent of the additional control group. The additional control group is included in the figures on the meta-analysis.
Thirteen independent studies in total were included in the meta-analysis. Five used randomizations (nos. 1, 3, 8, 9, 10), while the others employed a convenience sample. The weighted average of the follow-up time was almost 24 weeks (range: 6 weeks to 2 years).
Across all studies, the regression analysis indicated that time had no significant effect on the stability of the follow-up results, meaning that retention of learned knowledge and improvement in attitudes (including the desire for social distance) seemed stable over the measured time period.
The non-significant results of the meta-regression indicated that the intervention type (contact plus education, education, and unspecified) neither affected stigmatizing attitudes nor the desire for social distance at post- and follow-up assessment. The MHL outcomes, however, were significantly worse for the contact-based intervention compared to the educational intervention at post-assessment [β = −0.84; 95% CI = (−1.51, −0.16); SE = 0.35; p < 0.05] and at follow-up [β = −0.46, 95% CI = (− 0.87, −0.04); SE = 0.21, p < 0.05]. The unknown study type also showed significantly worse outcomes at post-assessment [β = −1.02; 95% CI = (−1.66, −0.38); SE = 0.33; p < 0.01].
At post-measurement, RCTs obtained significantly lower scores than other study designs for stigmatizing attitudes [β = −0.27; 95% CI = (−0.52, −0.02); SE = 0.13; p < 0.05], social distance [β = −0.26, 95% CI = (−0.49, −0.04), SE = 0.11, p < 0.05] and MHL [β = −0.67, 95% CI = (−1.08, −0.26), SE = 0.21, p = 0.001]. At follow-up, RCTs had significantly lower results only for MHL [β = −0.39, 95% CI = (−0.66, −0.13), SE = 0.13, p < 0.01], while no significant effect of study design could be observed for stigmatizing attitudes and social distance.
Mental Health Literacy
We were able to use data from eight studies, including 3,979 participants, to assess the immediate efficacy of interventions on MHL, as well as seven studies, including 3,522 participants, for the long-term follow-up (see Figure 2). The interventions could significantly improve MHL immediately after the intervention (one to 2 weeks afterwards) [d = 0.62, 95% CI = (0.34, 0.91)]. These effects diminished slightly over time (average of 23.62 weeks, range 6–25.8 weeks), but remained significant with a medium effect size [d = 0.48, 95% CI = (0.34, 0.62)] (see Figure 2). At both times, high heterogeneity was observed across studies: 94.44% at post-assessment and 71.51% at follow-up. Two studies showed negative, but not significant results at post- and follow-up assessment.
FIGURE 2
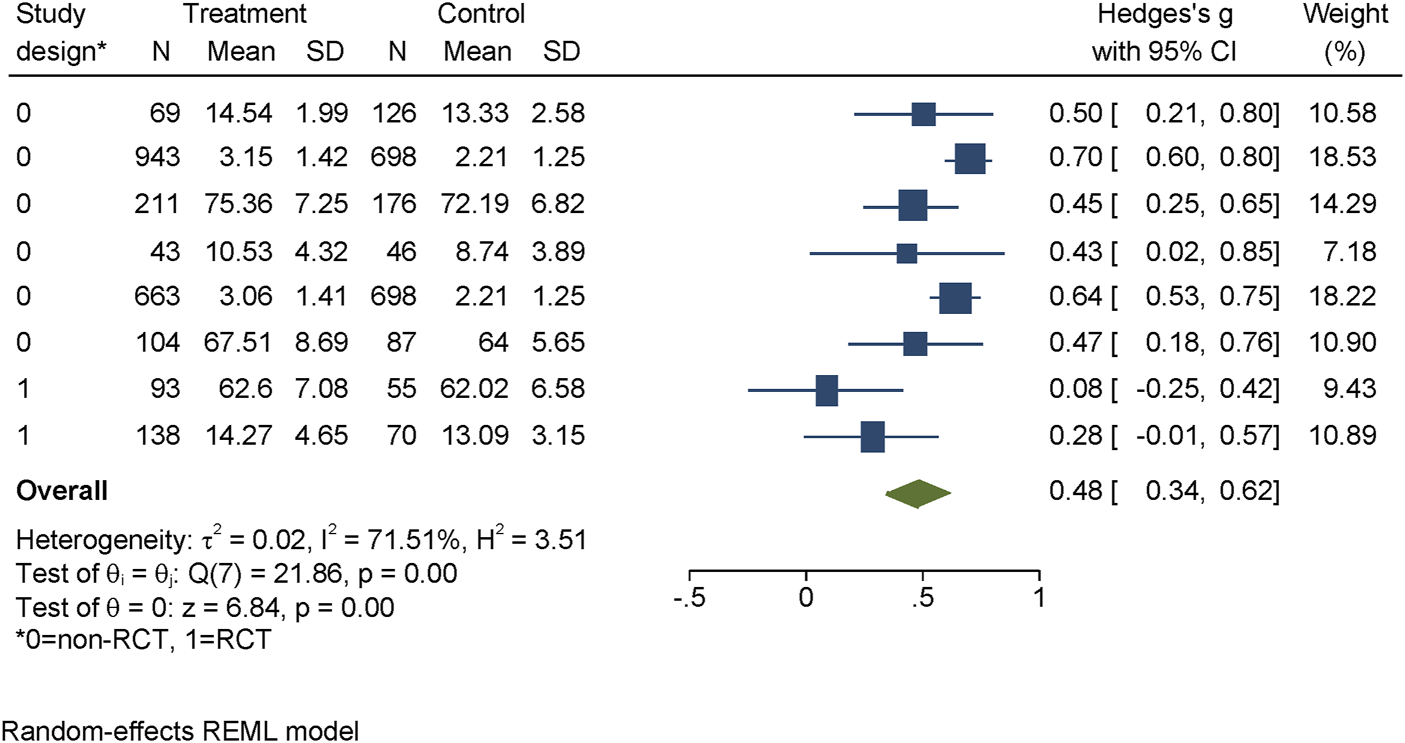
Evidence for effectiveness of interventions to improve MHL at follow-up assessment identified within the review regarding the effectiveness of long-term interventions addressing mental health literacy and stigma of mental illness in children and adolescents, search period: January 1997 to May 2020. Project: Improving mental health literacy to reduce stigma (IMPRES), Bielefeld, Germany, 03.2018 - 02.2021.
Stigmatizing Attitudes
Stigmatizing attitudes were measured by ten studies (including 4,272 participants) at post-assessment and nine studies (including 3,710 participants) at follow-up. The post-measurement was homogenous (one to 2 weeks after intervention) for all but one study, which first assessed the program after 52 weeks post-intervention. The average follow-up period was 23.62 weeks (range between 6 and 103 weeks). The interventions showed stable improvement over time, with effect sizes of d = 0.30, 95% CI = (0.17, 0.43) at post-assessment and d = 0.30, 95% CI = (0.24; 0.36) at follow-up (see Figure 3). At post-test, three studies, all RCTs, showed non-significant improvements of stigmatizing attitudes, while the others were significant. At follow-up, two-thirds of the studies showed positive, non-significant improvements. Only two of these, however, were RCTs. Moreover, one single study split into two conditions accounts for considerably more weight (68.83%) of the results in the follow-up. While the heterogeneity was high at post-assessment (I2 = 74.13%), at follow-up, it was 0.00%.
FIGURE 3
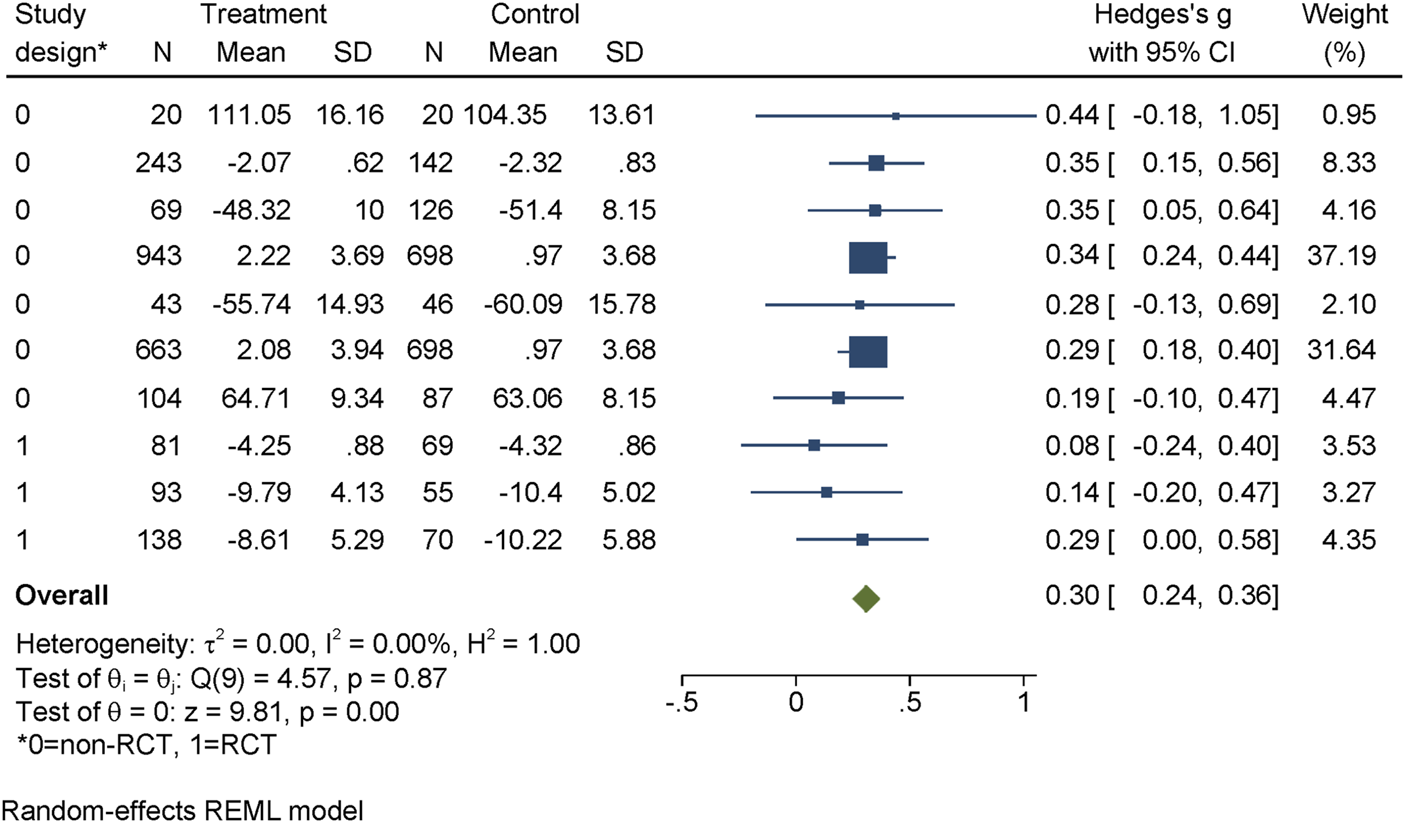
Evidence for effectiveness of interventions to reduce stigmatizing attitudes at follow-up assessment identified within the review regarding the effectiveness of long-term interventions addressing mental health literacy and stigma of mental illness in children and adolescents, search period: January 1997 to May 2020. Project: Improving mental health literacy to reduce stigma (IMPRES), Bielefeld, Germany, 03.2018 - 02.2021.
Social Distance
Six studies assessed social distance at post-assessment with 2908 participants and four at follow-up with 921 participants. The post-measurement was homogenous (usually 1 week after intervention) for all but one study, which first assessed the program after 52 weeks post-intervention. The average time until follow-up was almost 38 weeks (range from 6 to 103 weeks). Slight improvements were observed at post-intervention [d = 0.14, 95% CI = (0.02; 0.25)], and at follow-up [d = 0.16, 95% CI = (0.03, 0.29)] (see Figure 4). The heterogeneity at post-test was 17.74% and zero at follow-up. The non-significant studies outnumbered the significant ones: four out of six at post-test and three out of four at follow-up.
FIGURE 4
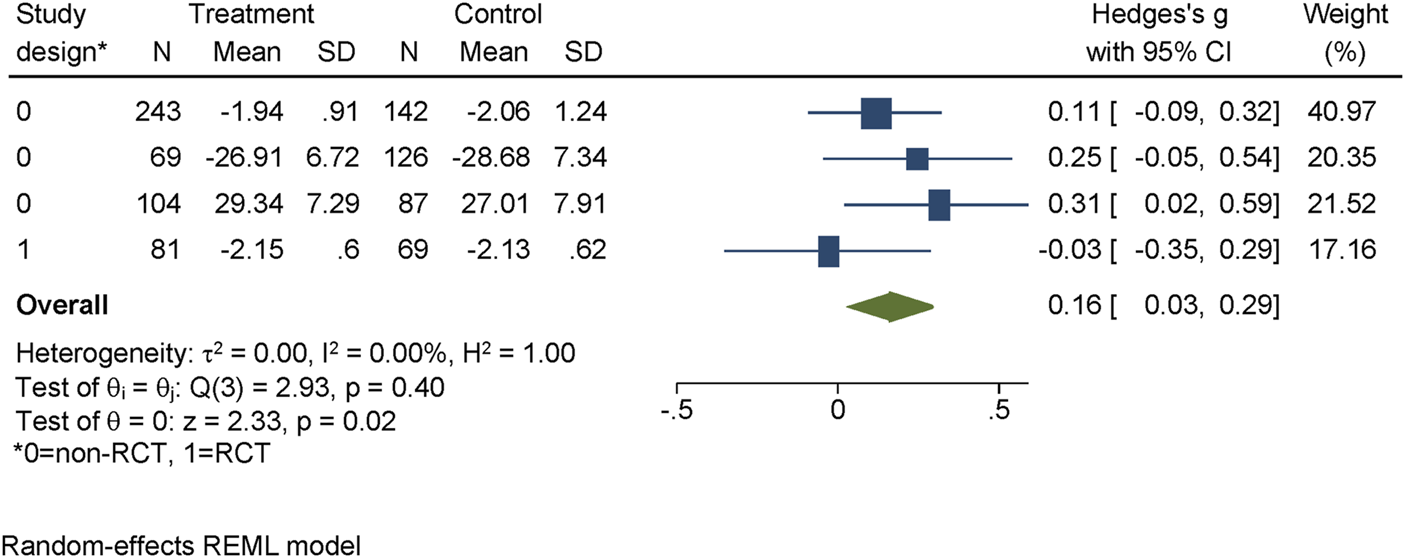
Evidence for effectiveness of interventions to reduce social distance at follow-up identified within the review regarding the effectiveness of long-term interventions addressing mental health literacy and stigma of mental illness in children and adolescents, search period: January 1997 to May 2020. Project: Improving mental health literacy to reduce stigma (IMPRES), Bielefeld, Germany, 03.2018 - 02.2021.
Discussion
To our knowledge, this is the first study considering interventions aiming at the long-term reduction of stigma or improvement of MHL in children or adolescents. We found 25 controlled follow-up studies addressing either MHL, stigma, or both. Interventions typically took place in a school setting and were mostly implemented in the span of up to 1 week, with up to 9 h.
In some cases, content was delivered by staff external to schools (e.g., mental health professionals, researchers, etc.) and by teachers themselves in others. One comparative study found that knowledge and attitudes improved when both professionals and teachers delivered the intervention [30]. Matching previous recommendations [45–49], interventions involving school staff within a school setting could still be a convenient and effective option.
It is also relevant to consider the complexity of an intervention’s content. We found that most studies tackled mental health and mental illness as a general topic, while others focused on particularly common mental illnesses (e.g., depression) [50], or particularly stigmatized illnesses (e.g., schizophrenia) [51]. While learning about specific aspects regarding incidence, symptoms, and treatments of a particular illness is relevant, we argue that tapping into more general aspects, such as the stigma surrounding mental illness and strategies related to resilience and positive mental health, is just as relevant. To our knowledge, however, no study exists comparing the effectiveness of interventions addressing general mental health with those addressing specific mental illnesses.
Overall results indicate a positive stable improvement of MHL and, to a smaller degree, stigmatizing attitudes and social distance. As was the case in a review targeting long-term results in adults, we found that effect sizes for knowledge retention were higher than for attitudinal change [52]. The evidence is less clear for long-term effectiveness regarding stigma and social distance, since most of the included studies showed non-significant improvements in these areas. More research is needed in this respect, especially in identifying which conditions (e.g., content, person who delivers intervention, intervention setting, duration, etc.) lead to better outcomes. Put differently, although the evidence indicates overall that exposure to or engagement with information about mental health leads to improved MHL and slightly more positive attitudes related to mental illness, further research should go beyond asking whether interventions are effective and instead ask which components make some more effective than others.
In this respect, we found that educational interventions contributed to significantly improved knowledge retention over educational plus contact interventions. One randomized trial identified within this review, which was excluded from the meta-analysis due to lack of a control group, compared an educational intervention to an educational plus contact intervention. The content of both education parts was the same except for a short input on the history of mental illness, which replaced the personal contact. Despite the high content overlap, the education condition proved more effective than the education plus contact condition in improving MHL (recognizing a mental illness based on a vignette) and knowledge, but not stigmatizing attitudes. However, the education plus contact condition did not lead to significant improvement of stigmatizing attitudes over the education condition [38]. Our meta-analysis showed the same trend: results observed for stigma variables in the education condition were not significantly worse than the education plus contact condition. This is somewhat surprising compared to previous findings, since one review has shown that for adolescents (differently than for adults), educational interventions are more effective in reducing stigma than contact interventions [16]. Comparative studies, such as that conducted by Chisholm et al. [38] are necessary to identify which intervention components improve which particular areas of MHL.
Regarding outcomes, the mean duration between intervention and follow-up was almost five and a half months across all studies included in the meta-analysis, ranging from 6 weeks to 2 years. Surprisingly, longer durations until follow-up were unrelated to worse results, indicating stability of knowledge retention and attitudinal change. Thus, we can assume that the results might be stable across the studies’ identified ranges up to a maximum of 2 years. More research is needed to verify what happens beyond this time frame and whether repeated future interventions are needed to maintain positive change.
Limitations
In the second search phase, only one of the researchers assessed study eligibility, which could lead to slightly biased results. Since a high agreement rate was reached within the first phase, however, we consider the risk of bias to be low.
Most identified studies reported positive significant results. This could be an indication of publication bias, especially related to the “file drawer problem” and thus overestimation of the identified effects. It has been estimated that publication bias can overestimate the treatment effect by up to 12% [53]. However, since our analytic method (random effect models) provides a more conservative estimate of the combined data [54], the bias in the obtained results might be limited.
Despite our focus on long-term follow-ups, outcome measurements took place, on average, 5 months after the intervention, making estimation of what happens beyond this time frame impossible. Thus, it is necessary to determine how long results are sustained by using longer follow-up periods, and whether one implemented intervention is sufficient or if the aim should be to repeat interventions regularly.
Another limiting aspect involves outcome categorization. The studies’ usages of different measurement tools for the same constructs renders them not readily comparable. We tried carefully assigning each outcome to the most appropriate category to reduce heterogeneity stemming from differences in outcome operationalization. Still, the MHL meta-analysis revealed high heterogeneity, both at post and follow-up assessment, while high heterogeneity across studies investigating stigma was only present at post-test. This is partially explainable by the regression analysis: the MHL results were influenced by study designs (RCT vs. non-RCT) and intervention types at both time points, while for stigma, the results were only influenced by the study design and not intervention type at only one of the measurement time points. High heterogeneity might be connected to other factors, such as content variability and intervention duration, measurement tool variability, and the target population. Overall, generalizability of the results must be considered critically and intervention program application should, preferably, be accompanied by evaluations.
Additionally, the overall risk of bias assessment indicated that most studies show high or moderate risks, while few have a low risk. The rather unfavorable assessment is partly based on the fact that studies do not report on all assessed aspects. We recommend that intervention studies follow reporting guidelines to overcome this information gap and offer more reliable results. In terms of randomization, as one of the used quality criterion, the great majority (11 of 13 studies) were randomized at a group level, most of which were school classes, while the rest were randomized at an individual level. Cluster randomized studies, where randomization takes place at a group level, require a larger sample size for reaching acceptable power to reveal significant results [55]. Thus, due to the inclusion of cluster-randomized studies, the results may be underestimated. Moreover, differences in results can occur due to the type of cluster chosen. Randomization at school level may also lead to underestimation of the results due to possible contamination bias, when pupils from different classes exchange information received within the intervention.
Conclusion
We found 25 studies on interventions addressing MHL or stigma with varying content, delivery, and follow-up lengths. Schools were the predominant setting of delivery, where topics addressed were general mental health, depression, and schizophrenia. The meta-analysis indicates that interventions appear successful in improving MHL in the long term but provide less robust information on improving attitudes. We found that stigma and social distance did not vary across different intervention types, however, the education condition led to better MHL outcomes than the education plus contact condition. More studies are needed to identify which information should be conveyed in what way in order to successfully address both MHL and different aspects of stigma.
Statements
Author contributions
Planning manuscript: AF, PG, and UB. Writing manuscript: AF, SK, GG, and TB. Data extraction and selection: AF, SK, and PG. Data analysis: OS. Data visualization: AF, SK, and GG. Proofread: OS and UB.
Funding
We acknowledge support for the publication costs by the Open Access Publication Fund of Bielefeld University. The project has been funded by the Ministry of Education and Research in Germany, as part of the Health Literacy in Childhood and Adolescence research consortium (grant number: 01EL1824A).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2021.1604072/full#supplementary-material
References
1.
Kessler RC Berglund P Demler O Jin R Merikangas KR Walters EE . Lifetime Prevalence and Age-Of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry (2005) 62(6):593–602. 10.1001/archpsyc.62.6.593
2.
Patel V Flisher AJ Hetrick S McGorry P . Mental Health of Young People: a Global Public-Health challenge. The Lancet (2007) 369(9569):1302–13. 10.1016/s0140-6736(07)60368-7
3.
Goodman A Joyce R Smith JP . The Long Shadow Cast by Childhood Physical and Mental Problems on Adult Life. Proc Natl Acad Sci (2011) 108(15):6032–7. 10.1073/pnas.1016970108
4.
Wainberg ML Scorza P Shultz JM Helpman L Mootz JJ Johnson KA et al Challenges and Opportunities in Global Mental Health: a Research-To-Practice Perspective. Curr Psychiatry Rep (2017) 19(5):28. 10.1007/s11920-017-0780-z
5.
Jorm AF Korten AE Jacomb PA Christensen H Rodgers B Pollitt P . "Mental Health Literacy": a Survey of the Public's Ability to Recognise Mental Disorders and Their Beliefs about the Effectiveness of Treatment. Med J Aust (1997) 166(4):182–6. 10.5694/j.1326-5377.1997.tb140071.x
6.
Bonabi H Müller M Ajdacic-Gross V Eisele J Rodgers S Seifritz E et al Mental Health Literacy, Attitudes to Help Seeking, and Perceived Need as Predictors of Mental Health Service Use. J Nerv Ment Dis (2016) 204(4):321–4. 10.1097/nmd.0000000000000488
7.
Tully LA Hawes DJ Doyle FL Sawyer MG Dadds MR . A National Child Mental Health Literacy Initiative Is Needed to Reduce Childhood Mental Health Disorders. Aust N Z J Psychiatry (2019) 53(4):286–90. 10.1177/0004867418821440
8.
Sickel AE Seacat JD Nabors NA . Mental Health Stigma Update: A Review of Consequences. Adv Ment Health (2014) 12(3):202–15. 10.1080/18374905.2014.11081898
9.
Corrigan PW . Mental Health Stigma as Social Attribution: Implications for Research Methods and Attitude Change. Clin Psychol Sci Pract (2000) 7(1):48–67. 10.1093/clipsy.7.1.48
10.
Corrigan PW Watson AC . The Paradox of Self-Stigma and Mental Illness. Clin Psychol Sci Pract (2002) 9(1):35–53. 10.1093/clipsy.9.1.35
11.
Rüsch N Angermeyer MC Corrigan PW . Mental Illness Stigma: Concepts, Consequences, and Initiatives to Reduce Stigma. Eur Psychiatr (2005) 20(8):529–39. 10.1016/j.eurpsy.2005.04.004
12.
Schomerus G Schwahn C Holzinger A Corrigan PW Grabe HJ Carta MG et al Evolution of Public Attitudes about Mental Illness: a Systematic Review and Meta-Analysis. Acta Psychiatr Scand (2012) 125(6):440–52. 10.1111/j.1600-0447.2012.01826.x
13.
O'Reilly M Svirydzenka N Adams S Dogra N . Review of Mental Health Promotion Interventions in Schools. Soc Psychiatry Psychiatr Epidemiol (2018) 53(7):647–62. 10.1007/s00127-018-1530-1
14.
Gronholm PC Henderson C Deb T Thornicroft G . Interventions to Reduce Discrimination and Stigma: the State of the Art. Soc Psychiatry Psychiatr Epidemiol (2017) 52(3):249–58. 10.1007/s00127-017-1341-9
15.
Thornicroft G Mehta N Clement S Evans-Lacko S Doherty M Rose D et al Evidence for Effective Interventions to Reduce Mental-Health-Related Stigma and Discrimination. Lancet (2015) 387(10023):1123–32. 10.1016/S0140-6736(15)00298-6
16.
Corrigan PW Morris SB Michaels PJ Rafacz JD Rüsch N . Challenging the Public Stigma of Mental Illness: A Meta-Analysis of Outcome Studies. Psychiatr. Serv. (2012) 63(10):963–973. 10.1176/appi.ps.201100529
17.
Wei Y Hayden JA Kutcher S Zygmunt A McGrath P . The Effectiveness of School Mental Health Literacy Programs to Address Knowledge, Attitudes and Help Seeking Among Youth. Early Intervention in Psychiatry (2013) 7(2):109–21. 10.1111/eip.12010
18.
Seedaket S Turnbull N Phajan T Wanchai A . Improving Mental Health Literacy in Adolescents: Systematic Review of Supporting Intervention Studies. Trop Med Int Health (2020) 25(9):1055–64. 10.1111/tmi.13449
19.
Patafio B Miller P Baldwin R Taylor N Hyder S . A Systematic Mapping Review of Interventions to Improve Adolescent Mental Health Literacy, Attitudes and Behaviours. Early Intervention in Psychiatry (2021). 10.1111/eip.13109
20.
Spiker DA Hammer JH . Mental Health Literacy as Theory: Current Challenges and Future Directions. J Ment Health (2018) 28(3):238–42. 10.1080/09638237.2018.1437613
21.
National Hearth, Blood and Lung Institute. Checklist for Quality Assessment of Controlled Intervention Studies. Internet. Available from: URL: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (Accessed 8, 2021).
22.
Stata Statistical Software. Release 16. College Station, TX: StataCorp LLC (2019).
23.
Sedgwick P . Meta-analyses: what Is Heterogeneity?BMJ (2015) 350:h1435. 10.1136/bmj.h1435
24.
Ahmad SI Leventhal BL Nielsen BN Hinshaw SP . Reducing Mental-Illness Stigma via High School Clubs: A Matched-Pair, Cluster-Randomized Trial. Stigma and Health (2020) 5(2):230–9. 10.1037/sah0000193
25.
Andrés-Rodríguez L Pérez-Aranda A Feliu-Soler A Rubio-Valera M Aznar-Lou I Serrano-Blanco A et al Effectiveness of the "What's up!" Intervention to Reduce Stigma and Psychometric Properties of the Youth Program Questionnaire (YPQ): Results from a Cluster Non-randomized Controlled Trial Conducted in Catalan High Schools. Front Psychol (2017) 8:1608. 10.3389/fpsyg.2017.01608
26.
Campos L Dias P Duarte A Veiga E Dias C Palha F . Is it Possible to "Find Space for Mental Health" in Young People? Effectiveness of a School-Based Mental Health Literacy Promotion Program. Ijerph (2018) 15(7):1426. 10.3390/ijerph15071426
27.
Esters IG Cooker PG Ittenbach RF . Effects of a Unit of Instruction in Mental Health on Rural Adolescents' Conceptions of Mental Illness and Attitudes about Seeking Help. Adolescence (1998) 33(130):469–76.
28.
Fraser E Pakenham KI . Evaluation of a Resilience-Based Intervention for Children of Parents with Mental Illness. Aust N Z J Psychiatry (2008) 42(12):1041–50. 10.1080/00048670802512065
29.
Ibrahim N Mohd Safien A Siau CS Shahar S . The Effectiveness of a Depression Literacy Program on Stigma and Mental Help-Seeking Among Adolescents in Malaysia: A Control Group Study with 3-Month Follow-Up. Inquiry (2020) 57:46958020902332. 10.1177/0046958020902332
30.
Lai ESY Kwok C-L Wong PWC Fu K-W Law Y-W Yip PSF . The Effectiveness and Sustainability of a Universal School-Based Programme for Preventing Depression in Chinese Adolescents: A Follow-Up Study Using Quasi-Experimental Design. PLoS ONE (2016) 11(2):e0149854. 10.1371/journal.pone.0149854
31.
Morgan AJ Fischer J-AA Hart LM Kelly CM Kitchener BA Reavley NJ et al Does Mental Health First Aid Training Improve the Mental Health of Aid Recipients? the Training for Parents of Teenagers Randomised Controlled Trial. BMC Psychiatry (2019) 19(1):99. 10.1186/s12888-019-2085-8
32.
Perry Y Petrie K Buckley H Cavanagh L Clarke D Winslade M et al Effects of a Classroom-Based Educational Resource on Adolescent Mental Health Literacy: A Cluster Randomised Controlled Trial. J Adolescence (2014) 37(7):1143–51. 10.1016/j.adolescence.2014.08.001
33.
Pinto-Foltz MD Logsdon MC Myers JA . Feasibility, Acceptability, and Initial Efficacy of a Knowledge-Contact Program to Reduce Mental Illness Stigma and Improve Mental Health Literacy in Adolescents. Soc Sci Med (2011) 72(12):2011–9. 10.1016/j.socscimed.2011.04.006
34.
Robinson J Gook S Yuen HP Hughes A Dodd S Bapat S et al Depression Education and Identification in Schools: An Australian-based Study. Sch Ment Health (2010) 2(1):13–22. 10.1007/s12310-009-9022-9
35.
Ventieri D Clarke DM Hay M . The Effects of a School-Based Educational Intervention on Preadolescents' Knowledge of and Attitudes towards Mental Illness. Adv Sch Ment Health Promot (2011) 4(3):5–17. 10.1080/1754730x.2011.9715632
36.
Wahl OF Susin J Kaplan L Lax A Zatina D . Changing Knowledge and Attitudes with a Middle School Mental Health Education Curriculum. Stigma Res Action (2011) 1(1):44–53. 10.5463/sra.v1i1.17
37.
Campbell M Shryane N Byrne R Morrison AP . A Mental Health Promotion Approach to Reducing Discrimination about Psychosis in Teenagers. Psychosis (2010) 3(1):41–51.
38.
Chisholm K Patterson P Torgerson C Turner E Jenkinson D Birchwood M . Impact of Contact on Adolescents' Mental Health Literacy and Stigma: the SchoolSpace Cluster Randomised Controlled Trial. BMJ Open (2016) 6(2):e009435. 10.1136/bmjopen-2015-009435
39.
Conrad I Dietrich S Heider D Blume A Angermeyer MC Riedel‐Heller S . "Crazy? So what!":Health Edu (2009) 109(4):314–28. 10.1108/09654280910970893
40.
Economou M Louki E Peppou LE Gramandani C Yotis L Stefanis CN . Fighting Psychiatric Stigma in the Classroom: the Impact of an Educational Intervention on Secondary School Students' Attitudes to Schizophrenia. Int J Soc Psychiatry (2011) 58(5):544–51. 10.1177/0020764011413678
41.
Gonçalves M Moleiro C Cook B . The Use of a Video to Reduce Mental Health Stigma Among Adolescents. APS (2015) 5(3):204–11. 10.2174/2210676605666150521232049
42.
Hart LM Cropper P Morgan AJ Kelly CM Jorm AF . Teen Mental Health First Aid as a School-Based Intervention for Improving Peer Support of Adolescents at Risk of Suicide: Outcomes from a Cluster Randomised Crossover Trial. Aust N Z J Psychiatry (2019) 54(4):382–92. 10.1177/0004867419885450
43.
Liddle SK Deane FP Batterham M Vella SA . A Brief Sports-Based Mental Health Literacy Program for Male Adolescents: A Cluster-Randomized Controlled Trial. J Appl Sport Psychol (2021) 33(1):20–44. 10.1080/10413200.2019.1653404
44.
Mulfinger N Müller S Böge I Sakar V Corrigan PW Evans-Lacko S et al Honest, Open, Proud for Adolescents with Mental Illness: Pilot Randomized Controlled Trial. J Child Psychol Psychiatr (2018) 59(6):684–91. 10.1111/jcpp.12853
45.
Ng P Chan K-F . Attitudes towards People with Mental Illness. Effects of a Training Program for Secondary School Students. Int J Adolesc Med Health (2002) 14(3):215–24. 10.1515/ijamh.2002.14.3.215
46.
Schulze B Richter-Werling M Matschinger H Angermeyer MC . Crazy? So what! Effects of a School Project on Students' Attitudes towards People with Schizophrenia. Acta Psychiatr Scand (2003) 107(2):142–50. 10.1034/j.1600-0447.2003.02444.x
47.
Swartz K Musci RJ Beaudry MB Heley K Miller L Alfes C et al School-Based Curriculum to Improve Depression Literacy Among US Secondary School Students: A Randomized Effectiveness Trial. Am J Public Health (2017) 107(12):1970–6. 10.2105/ajph.2017.304088
48.
Wahl O Rothman J Brister T Thompson C . Changing Student Attitudes about Mental Health Conditions: NAMI Ending the Silence. Stigma and Health (2018) 4(2):188–95.
49.
Yap MBH Mackinnon A Reavley N Jorm AF . The Measurement Properties of Stigmatizing Attitudes towards Mental Disorders: Results from Two Community Surveys. Int J Methods Psychiatr Res (2014) 23(1):49–61. 10.1002/mpr.1433
50.
Liu Q He H Yang J Feng X Zhao F Lyu J . Changes in the Global burden of Depression from 1990 to 2017: Findings from the Global Burden of Disease Study. J Psychiatr Res (2020) 126:134–40. 10.1016/j.jpsychires.2019.08.002
51.
Reavley N Too T Zhao M . National Surveys of Mental Health Literacy and Stigma and National Survey of Discrimination and Positive Treatment: A Report for the Mental Health Commission of NSW. Sydney: Mental Health Commission of NSW (2015).
52.
Mehta N Clement S Marcus E Stona A-C Bezborodovs N Evans-Lacko S et al Evidence for Effective Interventions to Reduce Mental Health-Related Stigma and Discrimination in the Medium and Long Term: Systematic Review. Br J Psychiatry (2015) 207(5):377–84. 10.1192/bjp.bp.114.151944
53.
Moher D Cook DJ Eastwood S Olkin I Rennie D Stroup DF . Improving the Quality of Reports of Meta-Analyses of Randomised Controlled Trials: the QUOROM Statement. The Lancet (1999) 354:1896–900. 10.1016/s0140-6736(99)04149-5
54.
Russo MW . How to Review a Meta-Analysis. Gastroenterol Hepatol (N Y) (2007) 3(8):637–42.
55.
Dreyhaupt J Mayer B Keis O Öchsner W Muche R . Cluster-randomized Studies in Educational Research: Principles and Methodological Aspects. GMS J Med Educ (2017) 34(2):Doc26. 10.3205/zma001103
Summary
Keywords
adolescents, long-term effectiveness, mental health literacy, stigma, social distance, intervention, mental illness
Citation
Freţian AM, Graf P, Kirchhoff S, Glinphratum G, Bollweg TM, Sauzet O and Bauer U (2021) The Long-Term Effectiveness of Interventions Addressing Mental Health Literacy and Stigma of Mental Illness in Children and Adolescents: Systematic Review and Meta-Analysis. Int J Public Health 66:1604072. doi: 10.3389/ijph.2021.1604072
Received
06 March 2021
Accepted
01 November 2021
Published
15 December 2021
Volume
66 - 2021
Edited by
Sibel Sakarya, Koç University, Turkey
Reviewed by
Eilis Hennessy, University College Dublin, Ireland
Stolzenburg Stolzenburg, Helios Hanseklinikum, Germany
Updates
Copyright
© 2021 Freţian, Graf, Kirchhoff, Glinphratum, Bollweg, Sauzet and Bauer.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alexandra Maria Freţian, fretian@uni-bielefeld.de
†ORCID ID:Alexandra Maria Freţianorcid.org/0000-0001-6268-6800
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.